Insulin resistance is a condition where your body’s cells become less responsive to insulin, a hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels. When you eat, your body breaks down carbohydrates into glucose, which enters your bloodstream. Insulin helps cells absorb this glucose to use it for energy or store it for later use.
However, when you develop insulin resistance, your cells do not respond effectively to insulin, leading to elevated blood sugar levels.
Understanding insulin resistance is essential because it is often a precursor to more serious health issues, including type 2 diabetes and cardiovascular diseases.
The condition can develop gradually and may go unnoticed for years, making it crucial for you to be aware of the risk factors and symptoms. By recognizing the signs early on, you can take proactive steps to manage your health and prevent further complications.
Key Takeaways
- Insulin resistance is a condition where the body’s cells do not respond properly to insulin, leading to high blood sugar levels.
- Causes and risk factors of insulin resistance include obesity, physical inactivity, genetics, and certain medical conditions.
- Symptoms of insulin resistance may include fatigue, increased thirst, frequent urination, and darkened skin patches.
- Diagnosis and testing for insulin resistance involve blood tests to measure glucose and insulin levels, as well as other markers of metabolic health.
- Complications of insulin resistance can include type 2 diabetes, heart disease, and polycystic ovary syndrome.
Causes and Risk Factors of Insulin Resistance
Several factors contribute to the development of insulin resistance, and understanding these can help you identify your own risk. One of the primary causes is obesity, particularly excess fat around the abdomen. When you carry extra weight, especially visceral fat, it can interfere with the way your body responds to insulin.
Additionally, a sedentary lifestyle can exacerbate this issue; lack of physical activity reduces your body’s ability to utilize insulin effectively. Genetics also play a significant role in insulin resistance. If you have a family history of diabetes or metabolic syndrome, your risk may be higher.
Other contributing factors include hormonal changes, such as those experienced during pregnancy or menopause, and certain medical conditions like polycystic ovary syndrome (PCOS). Furthermore, age is a factor; as you get older, your risk of developing insulin resistance increases due to changes in body composition and metabolism.
Symptoms of Insulin Resistance
Recognizing the symptoms of insulin resistance can be challenging since they often develop gradually and may not be immediately apparent. One common sign is fatigue; you may find yourself feeling unusually tired or sluggish after meals, as your body struggles to manage blood sugar levels effectively. Additionally, you might notice increased hunger or cravings, particularly for sugary or carbohydrate-rich foods, as your cells are not receiving the energy they need.
Other symptoms can include difficulty concentrating, often referred to as “brain fog,” and unexplained weight gain, especially around the abdomen. Skin changes may also occur; some individuals develop dark patches of skin known as acanthosis nigricans, typically found in areas like the neck or armpits. If you experience any of these symptoms consistently, it’s essential to consult with a healthcare professional for further evaluation.
Diagnosis and Testing for Insulin Resistance
| Diagnosis and Testing for Insulin Resistance |
|---|
| 1. Fasting Plasma Glucose Test |
| 2. Oral Glucose Tolerance Test (OGTT) |
| 3. Insulin Level Test |
| 4. Hemoglobin A1c Test |
| 5. Homeostasis Model Assessment (HOMA-IR) |
Diagnosing insulin resistance typically involves a combination of medical history assessment, physical examination, and laboratory tests. Your healthcare provider may start by asking about your symptoms, lifestyle habits, and family history of diabetes or metabolic disorders. A physical examination may reveal signs such as excess abdominal fat or skin changes associated with insulin resistance.
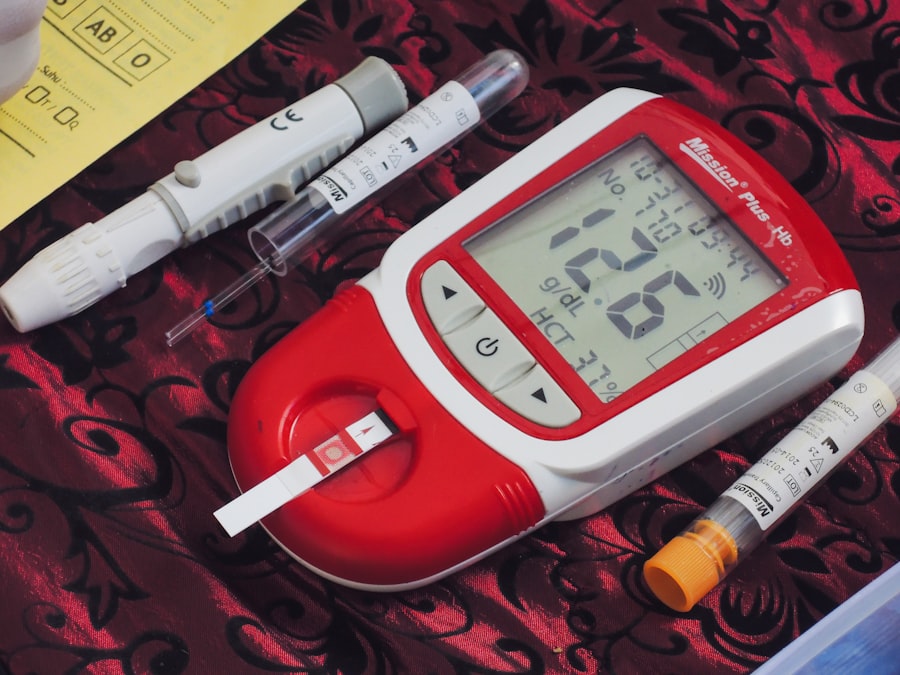
Laboratory tests are crucial for confirming the diagnosis. Common tests include fasting blood glucose levels and insulin levels. A fasting blood glucose test measures your blood sugar after an overnight fast; elevated levels may indicate insulin resistance.
Additionally, an oral glucose tolerance test (OGTT) can provide further insight into how your body processes glucose over time. In some cases, healthcare providers may also use the Homeostasis Model Assessment (HOMA-IR) to estimate insulin resistance based on fasting insulin and glucose levels.
Complications of Insulin Resistance
If left unaddressed, insulin resistance can lead to several serious health complications. One of the most significant risks is the development of type 2 diabetes. As your body continues to struggle with insulin sensitivity, blood sugar levels can rise to dangerous levels, leading to diabetes and its associated complications, such as nerve damage, kidney disease, and vision problems.
Beyond diabetes, insulin resistance is also linked to cardiovascular diseases. Elevated insulin levels can contribute to high blood pressure and abnormal cholesterol levels, increasing your risk of heart attack and stroke. Additionally, metabolic syndrome—a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels—often accompanies insulin resistance.
This syndrome significantly raises your risk for heart disease and other serious health issues.
Treatment and Management of Insulin Resistance

Managing insulin resistance typically involves a multifaceted approach that includes lifestyle modifications and medical interventions when necessary. The first line of treatment often focuses on making dietary changes and increasing physical activity. These adjustments can help improve your body’s sensitivity to insulin and lower blood sugar levels over time.
In some cases, healthcare providers may prescribe medications to help manage insulin resistance. Metformin is one commonly prescribed medication that helps improve insulin sensitivity and lower blood sugar levels. However, lifestyle changes remain crucial even when medications are involved; they work best in conjunction with a healthy diet and regular exercise.
Lifestyle Changes for Insulin Resistance
Making lifestyle changes is one of the most effective ways to combat insulin resistance. You might start by focusing on achieving a healthy weight if you’re overweight or obese. Even modest weight loss—around 5-10% of your total body weight—can significantly improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
Incorporating regular physical activity into your routine is equally important. Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, along with strength training exercises at least twice a week. These activities not only help with weight management but also enhance your body’s ability to use insulin effectively.
Diet and Nutrition for Insulin Resistance
Your diet plays a pivotal role in managing insulin resistance. Focus on consuming whole foods that are rich in nutrients while minimizing processed foods high in sugars and unhealthy fats. Incorporate plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats into your meals.
Foods high in fiber can be particularly beneficial as they help regulate blood sugar levels and improve overall gut health. Additionally, consider monitoring your carbohydrate intake. Opt for complex carbohydrates that are digested more slowly, such as whole grains and legumes, rather than simple sugars found in sugary snacks and beverages.
Balancing your meals with protein and healthy fats can also help stabilize blood sugar levels throughout the day.
Exercise and Physical Activity for Insulin Resistance
Regular exercise is one of the most effective strategies for improving insulin sensitivity. Engaging in aerobic activities like walking, jogging, cycling, or swimming can help lower blood sugar levels by increasing glucose uptake by muscles during physical activity. Aim for at least 30 minutes of moderate exercise most days of the week; this can be broken down into shorter sessions if needed.
Building muscle mass enhances your body’s ability to utilize glucose effectively and improves overall metabolism. Consider working with a fitness professional if you’re unsure where to start; they can help design a program tailored to your needs and fitness level.
Medications for Insulin Resistance
While lifestyle changes are foundational in managing insulin resistance, medications may be necessary for some individuals who struggle to achieve their goals through diet and exercise alone. Metformin is often the first-line medication prescribed; it works by decreasing glucose production in the liver and improving insulin sensitivity in muscle cells. Other medications may also be considered based on individual circumstances.
For instance, thiazolidinediones (TZDs) are another class of drugs that can enhance insulin sensitivity but may have side effects that need careful monitoring. Your healthcare provider will work with you to determine the most appropriate treatment plan based on your specific needs and health status.
Prevention of Insulin Resistance
Preventing insulin resistance is possible through proactive lifestyle choices that promote overall health and well-being. Maintaining a healthy weight through balanced nutrition and regular physical activity is key; even small changes can make a significant difference over time. Prioritizing sleep is also essential; poor sleep quality has been linked to increased insulin resistance.
Additionally, managing stress through mindfulness practices such as meditation or yoga can positively impact your metabolic health. By adopting these preventive measures early on, you can significantly reduce your risk of developing insulin resistance and its associated complications in the future. Remember that small steps taken consistently can lead to lasting changes in your health journey.
Insulin resistance is a condition where the body’s cells become less responsive to the hormone insulin, leading to elevated blood sugar levels and potentially progressing to type 2 diabetes. Understanding the implications of insulin resistance is crucial, especially for seniors who may be at a higher risk due to age-related factors. For more detailed information on managing health conditions like insulin resistance in older adults, you can explore this insightful article on senior health:
