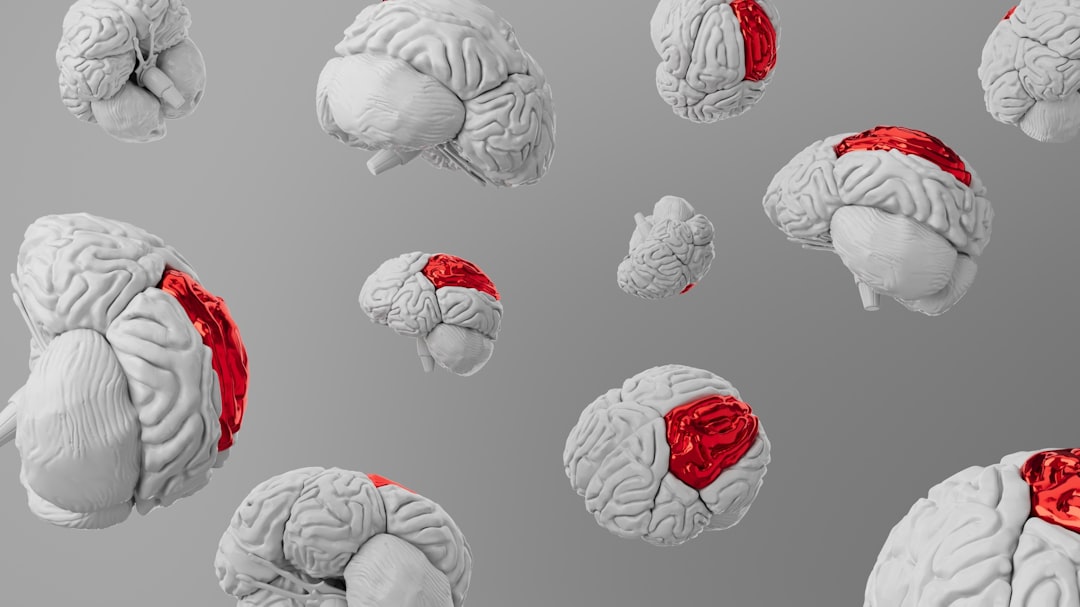
Anticholinergic cognitive burden (ACB) refers to the cumulative effect of medications that block the action of acetylcholine, a neurotransmitter crucial for various cognitive functions. As you delve into this topic, it becomes clear that ACB is not merely a side effect of certain drugs; it represents a significant concern, particularly for older adults. The aging population is often prescribed multiple medications, many of which may have anticholinergic properties.
This can lead to a heightened risk of cognitive decline, confusion, and other neurological issues. Understanding ACB is essential for both healthcare providers and patients, as it can influence treatment decisions and overall health outcomes. The implications of ACB extend beyond individual medications.
When you consider the polypharmacy often seen in older adults—where multiple drugs are prescribed simultaneously—the risk of cognitive impairment increases. This cumulative burden can lead to a range of symptoms, from mild forgetfulness to severe dementia-like conditions. Recognizing the signs and understanding the underlying mechanisms of ACB can empower you to engage in more informed discussions with healthcare professionals about your treatment options.
Key Takeaways
- Anticholinergic medications can impair cognitive function, especially in older adults, contributing to increased cognitive burden.
- Recent research highlights a significant link between long-term use of anticholinergic drugs and an elevated risk of dementia.
- Identifying and managing anticholinergic cognitive burden involves careful assessment and consideration of alternative treatments.
- Healthcare providers play a crucial role in educating patients and minimizing the cognitive risks associated with these medications.
- Ongoing research aims to better understand anticholinergic effects and develop safer therapeutic strategies for cognitive health.
The Impact of Anticholinergic Medications on Cognitive Function
Anticholinergic medications can significantly impact cognitive function, particularly in older adults whose brains may already be vulnerable due to age-related changes. When you take these medications, they can interfere with neurotransmission, leading to difficulties in memory, attention, and overall cognitive processing. Research has shown that even low doses of anticholinergic drugs can result in measurable declines in cognitive performance, which can be particularly concerning for those already at risk for cognitive decline.
Moreover, the effects of anticholinergic medications are not always immediately apparent. You might not notice changes in your cognitive function right away, but over time, the cumulative effects can become more pronounced. This gradual decline can lead to increased confusion, difficulty concentrating, and even mood changes.
Understanding how these medications affect your brain can help you make more informed choices about your health and well-being.
Identifying Anticholinergic Medications
Identifying anticholinergic medications is crucial for anyone concerned about cognitive health. Many common medications fall into this category, including certain antihistamines, antidepressants, and muscle relaxants. As you navigate your medication list, it’s important to be aware of which drugs may contribute to anticholinergic cognitive burden.
You might find it helpful to consult resources such as the Beers Criteria, which provides guidelines on potentially inappropriate medications for older adults. In addition to prescription medications, over-the-counter drugs can also have anticholinergic properties. For instance, some cold and allergy medications contain ingredients that can exacerbate cognitive decline.
By familiarizing yourself with these medications, you can take proactive steps to discuss alternatives with your healthcare provider. Being informed empowers you to advocate for your health and make choices that align with your cognitive well-being.
New Research Findings on Anticholinergic Cognitive Burden
Recent research has shed light on the complexities of anticholinergic cognitive burden and its long-term effects on brain health. Studies have indicated that prolonged use of anticholinergic medications may be linked to an increased risk of developing dementia and other neurodegenerative diseases. As you explore these findings, it becomes evident that the relationship between medication use and cognitive decline is multifaceted and requires careful consideration.
Moreover, new studies are examining the mechanisms behind ACB, seeking to understand how these medications affect brain structure and function over time. For instance, researchers are investigating how anticholinergic drugs may lead to changes in brain connectivity or contribute to neuroinflammation. These insights are crucial for developing strategies to mitigate the risks associated with anticholinergic medications and highlight the importance of ongoing research in this area.
The Link Between Anticholinergic Medications and Dementia
| Study | Sample Size | Population | Anticholinergic Burden Scale Used | Key Findings | Impact on Cognitive Function | Publication Year |
|---|---|---|---|---|---|---|
| Boustani et al. | 3,500 | Older adults (65+) | Anticholinergic Cognitive Burden (ACB) Scale | Higher ACB scores linked to increased risk of cognitive decline | Significant decline in memory and executive function | 2008 |
| Campbell et al. | 1,200 | Community-dwelling elderly | Anticholinergic Drug Scale (ADS) | Use of anticholinergic drugs associated with 2x risk of dementia | Increased risk of mild cognitive impairment | 2013 |
| Fox et al. | 13,000 | Older adults with normal cognition | Anticholinergic Cognitive Burden (ACB) Scale | Long-term use linked to accelerated cognitive decline | Decline in global cognitive scores over 5 years | 2014 |
| Ruxton et al. | 2,000 | Older adults in care homes | Anticholinergic Risk Scale (ARS) | High ARS scores correlated with poorer cognitive performance | Reduced attention and processing speed | 2015 |
| Gray et al. | 3,434 | Adults aged 65+ | Anticholinergic Cognitive Burden (ACB) Scale | Increased risk of dementia with cumulative anticholinergic exposure | Higher incidence of Alzheimer’s disease | 2015 |
The connection between anticholinergic medications and dementia is a growing area of concern among researchers and healthcare providers alike. As you consider this link, it’s important to recognize that while not all individuals who take anticholinergic drugs will develop dementia, there is a significant correlation that warrants attention. Studies have shown that individuals with a higher cumulative exposure to these medications are at an increased risk for developing dementia later in life.
Understanding this link can be particularly relevant if you or a loved one is taking multiple medications with anticholinergic properties. It may prompt you to engage in discussions with your healthcare provider about the necessity of each medication and explore potential alternatives. Being proactive about your medication management can play a crucial role in reducing your risk of cognitive decline and maintaining your overall health.
Managing Anticholinergic Cognitive Burden in Older Adults

Managing anticholinergic cognitive burden in older adults requires a multifaceted approach that involves careful medication review and lifestyle modifications. If you are an older adult or care for one, it’s essential to regularly assess the medications being taken and their potential impact on cognitive function. Collaborating with healthcare providers to create a comprehensive medication plan can help minimize the use of anticholinergic drugs while ensuring that necessary treatments are maintained.
In addition to medication management, lifestyle factors such as diet, exercise, and mental stimulation play a vital role in cognitive health. Engaging in regular physical activity, maintaining a balanced diet rich in antioxidants, and participating in activities that challenge your brain can help mitigate some of the cognitive risks associated with anticholinergic medications. By adopting a holistic approach to health management, you can take proactive steps toward preserving cognitive function as you age.
Assessing the Risk of Anticholinergic Medications in Cognitive Decline
Assessing the risk associated with anticholinergic medications involves evaluating both individual health factors and medication profiles. As you consider your own health or that of a loved one, it’s important to take into account pre-existing conditions that may heighten vulnerability to cognitive decline. For instance, individuals with a history of stroke or existing cognitive impairment may be at greater risk when taking anticholinergic drugs.
Additionally, regular assessments by healthcare providers can help identify potential risks early on. This may involve cognitive screenings or discussions about medication side effects during routine check-ups. By being proactive in assessing these risks, you can work collaboratively with healthcare professionals to make informed decisions about medication use and explore safer alternatives when necessary.
Alternative Treatment Options to Anticholinergic Medications
Exploring alternative treatment options is essential for those concerned about the cognitive effects of anticholinergic medications. Depending on the condition being treated, there may be non-anticholinergic alternatives available that provide similar benefits without the associated risks. For example, if you are taking an antihistamine for allergies, discussing non-sedating options with your healthcare provider could be beneficial.
In addition to pharmacological alternatives, lifestyle interventions such as cognitive behavioral therapy or mindfulness practices may offer effective solutions for managing conditions like anxiety or depression without resorting to anticholinergic medications. By considering a broader range of treatment options, you can work towards achieving better health outcomes while minimizing the risk of cognitive decline.
The Role of Healthcare Providers in Addressing Anticholinergic Cognitive Burden
Healthcare providers play a pivotal role in addressing anticholinergic cognitive burden through careful medication management and patient education. As a patient or caregiver, it’s important to engage actively with your healthcare team about any concerns regarding medications and their potential impact on cognitive health. Open communication can lead to more personalized care plans that prioritize both physical and mental well-being.
Moreover, healthcare providers should be vigilant in monitoring patients who are prescribed anticholinergic medications, especially older adults who may be more susceptible to their effects. Regular reviews of medication regimens can help identify opportunities for reducing or eliminating unnecessary anticholinergic drugs while ensuring that patients receive appropriate care for their medical conditions.
Educating Patients on Anticholinergic Cognitive Burden
Educating patients about anticholinergic cognitive burden is crucial for fostering awareness and promoting informed decision-making regarding medication use. As you learn more about this topic, consider discussing it with family members or friends who may also be affected by these issues. Sharing knowledge can empower others to advocate for their health and seek alternatives when necessary.
Healthcare providers should prioritize patient education by providing clear information about the risks associated with anticholinergic medications and encouraging patients to ask questions about their treatment plans.
Future Directions in Anticholinergic Cognitive Burden Research
The future of research on anticholinergic cognitive burden holds promise for uncovering new insights into its effects on brain health and developing strategies for prevention and management. As researchers continue to explore the mechanisms behind ACB, there is potential for identifying biomarkers that could predict susceptibility to cognitive decline related to medication use. Additionally, future studies may focus on developing guidelines for safer prescribing practices that minimize the use of anticholinergic medications while still addressing patients’ medical needs effectively.
By staying informed about ongoing research efforts in this area, you can remain proactive in managing your health and advocating for evidence-based approaches to medication management. In conclusion, understanding anticholinergic cognitive burden is essential for anyone concerned about cognitive health—especially older adults who may be taking multiple medications. By recognizing the impact of these drugs on cognitive function, identifying them within your medication regimen, and exploring alternative treatment options, you can take proactive steps toward preserving your mental well-being as you age.
Engaging with healthcare providers and educating yourself about this issue will empower you to make informed decisions that prioritize both physical and cognitive health.
Recent research has highlighted the significance of anticholinergic cognitive burden, particularly in older adults, as it can lead to increased risks of cognitive decline and dementia. A related article that delves deeper into this topic can be found at Explore Senior Health, where various studies and findings are discussed, providing valuable insights into the implications of anticholinergic medications on cognitive health.
🚨 WATCH THIS IF YOU TAKE ANY “PM” PILLS AFTER 60
FAQs
What is anticholinergic cognitive burden?
Anticholinergic cognitive burden refers to the cumulative effect of taking one or more medications that have anticholinergic properties, which can impair cognitive function, especially in older adults. These medications block the neurotransmitter acetylcholine, which is important for memory and learning.
Why is research on anticholinergic cognitive burden important?
Research is important because anticholinergic medications are commonly prescribed for various conditions, and their cognitive side effects can increase the risk of confusion, memory loss, dementia, and other cognitive impairments. Understanding this burden helps in safer prescribing practices and better patient outcomes.
Which medications contribute to anticholinergic cognitive burden?
Medications that contribute include certain antihistamines, antidepressants, antipsychotics, bladder antimuscarinics, and some Parkinson’s disease drugs. The degree of anticholinergic activity varies among these drugs.
Who is most at risk from anticholinergic cognitive burden?
Older adults are most at risk due to age-related changes in drug metabolism and increased sensitivity to anticholinergic effects. People with pre-existing cognitive impairment or dementia are also more vulnerable.
How is anticholinergic cognitive burden measured in research?
Researchers use scales such as the Anticholinergic Cognitive Burden Scale (ACB) or the Anticholinergic Drug Scale (ADS) to quantify the cumulative anticholinergic effect of a patient’s medication regimen.
Can anticholinergic cognitive burden be reduced?
Yes, by reviewing and adjusting medications to minimize or eliminate those with anticholinergic properties when possible, healthcare providers can reduce the cognitive burden and associated risks.
What are the potential cognitive effects of high anticholinergic burden?
Potential effects include memory impairment, confusion, decreased attention, increased risk of delirium, and a higher likelihood of developing dementia.
Is anticholinergic cognitive burden reversible?
Some cognitive effects may improve after discontinuing or reducing anticholinergic medications, but long-term or severe effects may not be fully reversible, especially in older adults.
How can patients discuss anticholinergic cognitive burden with their healthcare providers?
Patients should inform their providers about all medications they are taking, ask about the cognitive risks of their drugs, and discuss possible alternatives or dose adjustments to reduce anticholinergic burden.
What future directions does research on anticholinergic cognitive burden suggest?
Future research aims to better understand the mechanisms, identify safer medication alternatives, develop guidelines for prescribing, and explore interventions to mitigate cognitive risks associated with anticholinergic drugs.