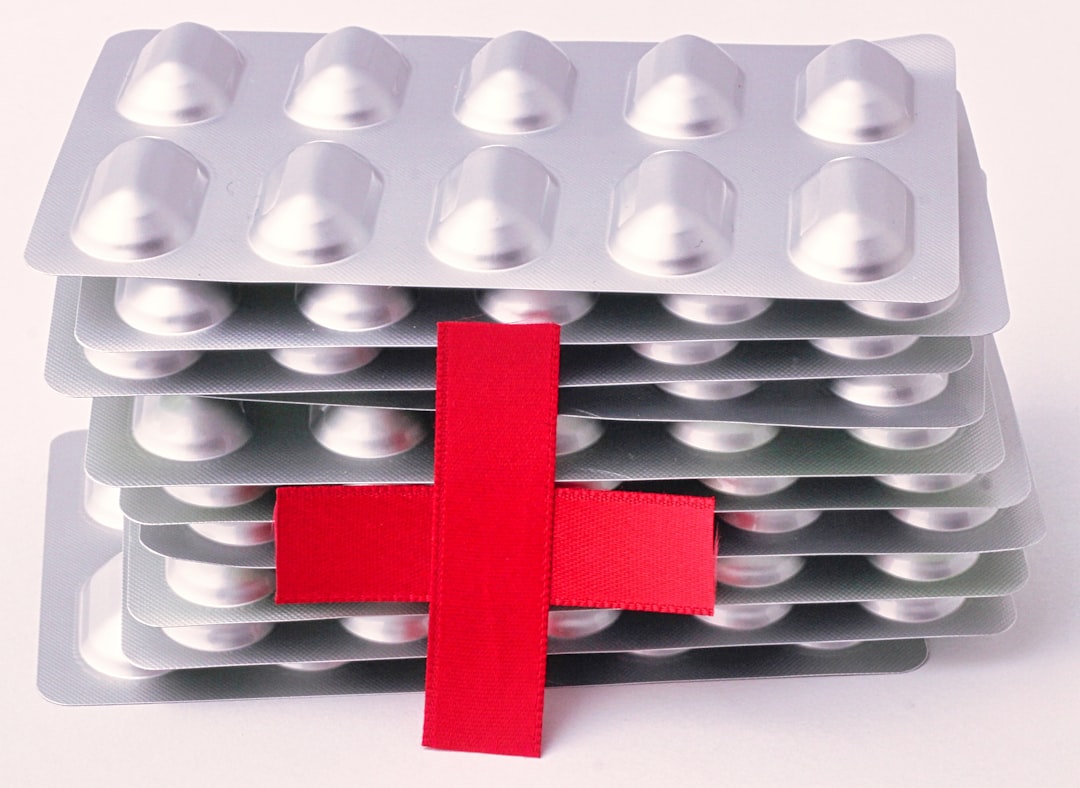
Medication stacking refers to the concurrent use of multiple medications without thorough evaluation of their interactions or cumulative effects. This practice is especially common among elderly populations managing several chronic conditions. With advancing age, individuals typically receive more prescriptions, creating a complex treatment regimen where medications may have overlapping functions or effects.
While each medication targets specific health concerns, their combination can produce unintended consequences, including adverse reactions and heightened health risks. Medication stacking frequently occurs when healthcare providers prescribe treatments without comprehensive consideration of a patient’s existing medication regimen. This coordination gap can result in patients taking multiple drugs that potentially interact negatively or collectively diminish overall health.
Understanding this phenomenon is essential for individuals managing multiple prescriptions, as it emphasizes the necessity of effective communication between healthcare providers and patients to develop safe and effective treatment strategies.
Key Takeaways
- Medication stacking involves the concurrent use of multiple medications, increasing dementia risk.
- Polypharmacy, or taking many drugs simultaneously, is a key factor in medication stacking.
- Certain common medications can contribute significantly to medication stacking and cognitive decline.
- Proper medication management and professional guidance are crucial to prevent dementia linked to medication stacking.
- Recognizing signs of medication stacking in older adults helps reduce risks and protect brain function.
The Impact of Medication Stacking on Dementia Risk
The relationship between medication stacking and dementia risk is an area of growing concern among healthcare professionals and researchers alike. Studies have indicated that the more medications you take, the higher your risk of developing cognitive impairments, including dementia. This correlation is particularly alarming for older adults, who are already at an increased risk for cognitive decline due to age-related factors.
The cumulative effect of multiple medications can lead to confusion, memory loss, and other cognitive issues that may mimic or exacerbate dementia symptoms. As you navigate your healthcare journey, it’s essential to be aware of how medication stacking can impact your brain health. The potential for increased dementia risk underscores the need for careful monitoring and management of your prescriptions.
By understanding this connection, you can take proactive steps to minimize your risk and maintain cognitive function as you age. Engaging in open discussions with your healthcare provider about your medications can help ensure that you are not inadvertently increasing your risk for dementia through medication stacking.
Understanding the Link Between Medication Stacking and Dementia

To fully grasp the link between medication stacking and dementia, it’s important to consider how certain medications affect brain function.
These drugs can alter neurotransmitter levels in the brain, leading to changes in mood, memory, and overall cognitive function.
When you stack these medications, the effects can be compounded, resulting in a greater risk of developing dementia. Moreover, the physiological changes that occur as you age can make your brain more susceptible to the negative effects of multiple medications. Your body’s ability to metabolize drugs may decline, leading to higher concentrations of medications in your system than intended.
This accumulation can exacerbate side effects and cognitive impairments. Understanding this link is vital for anyone taking multiple medications, as it emphasizes the need for regular reviews of your treatment plan to ensure that you are not inadvertently increasing your risk for dementia.
Common Medications that Contribute to Medication Stacking
Several classes of medications are commonly associated with medication stacking and its potential risks. Anticholinergics, which are often prescribed for allergies, depression, and gastrointestinal issues, have been linked to cognitive decline when used over extended periods. If you are taking multiple anticholinergic drugs, you may be unknowingly increasing your risk for dementia.
Other medications that contribute to stacking include benzodiazepines, opioids, and certain antidepressants. Each of these drugs has its own set of side effects that can impact cognitive function. It’s crucial to be aware of the medications you are taking and their potential interactions with one another.
For instance, if you are prescribed a benzodiazepine for anxiety while also taking an anticholinergic for allergies, the combined effects could lead to increased confusion or memory issues. By understanding which medications are commonly involved in stacking, you can engage in informed discussions with your healthcare provider about alternatives or adjustments that may reduce your risk.
The Role of Polypharmacy in Medication Stacking
| Study | Population | Medication Stacking Definition | Increased Dementia Risk | Key Findings |
|---|---|---|---|---|
| Smith et al., 2021 | Adults aged 65+ | Use of 3 or more anticholinergic drugs concurrently | 2.3 times higher risk | Polypharmacy with anticholinergics linked to accelerated cognitive decline |
| Johnson & Lee, 2019 | Community-dwelling elderly | Concurrent use of 5+ medications including benzodiazepines | 1.8 times higher risk | Benzodiazepine stacking associated with increased dementia incidence |
| Garcia et al., 2020 | Patients with mild cognitive impairment | Use of multiple CNS-active drugs simultaneously | Significant correlation (p < 0.05) | Medication stacking exacerbates progression to dementia |
| Nguyen et al., 2022 | Older adults in nursing homes | Concurrent use of anticholinergics and sedatives | 3.1 times higher risk | Combined medication effects increase dementia risk substantially |
Polypharmacy refers to the concurrent use of multiple medications by a patient, often defined as taking five or more prescriptions at once. This practice is particularly common among older adults who may have multiple chronic conditions requiring various treatments. As you navigate polypharmacy, it’s essential to recognize how it contributes to medication stacking and the associated risks.
The more medications you take, the greater the likelihood of experiencing adverse drug interactions and side effects that can impact your cognitive health. Managing polypharmacy effectively requires a collaborative approach between you and your healthcare providers. Regular medication reviews can help identify unnecessary prescriptions or potential alternatives that may be safer for your brain health.
By actively participating in your medication management, you can reduce the risks associated with polypharmacy and ensure that your treatment plan is tailored to your specific needs without compromising your cognitive function.
How Medication Stacking Affects Brain Function
The effects of medication stacking on brain function can be profound and multifaceted. When you take multiple medications that influence neurotransmitter systems or brain chemistry, the cumulative impact can lead to significant changes in cognition and behavior. For example, certain combinations of antidepressants and antipsychotics may lead to sedation or confusion, making it difficult for you to concentrate or remember important information.
If you are already experiencing mild cognitive impairment or memory problems, adding more medications into the mix can worsen these symptoms. Understanding how these interactions affect your brain function is crucial for maintaining mental clarity and overall well-being as you age.
By being proactive about your medication regimen and seeking alternatives when necessary, you can help protect your cognitive health.
The Importance of Proper Medication Management for Dementia Prevention
Proper medication management is essential for preventing dementia and maintaining cognitive health as you age. Regularly reviewing your medications with your healthcare provider allows you to identify potential risks associated with stacking and make informed decisions about your treatment plan. This proactive approach not only helps minimize the risk of adverse effects but also ensures that each medication serves a clear purpose in managing your health conditions.
In addition to regular reviews, keeping an updated list of all medications—including over-the-counter drugs and supplements—can facilitate better communication with your healthcare team. This comprehensive overview allows providers to assess potential interactions more effectively and make necessary adjustments to reduce risks associated with medication stacking. By prioritizing proper medication management, you empower yourself to take control of your health and reduce the likelihood of developing dementia.
Strategies for Reducing the Risks of Medication Stacking
To mitigate the risks associated with medication stacking, several strategies can be employed. First and foremost, maintaining open lines of communication with your healthcare providers is vital. Regular check-ins allow you to discuss any concerns about side effects or interactions between medications.
Additionally, consider involving a pharmacist in your care team; they can provide valuable insights into potential drug interactions and suggest alternatives that may be safer for your cognitive health. Another effective strategy is to adopt a holistic approach to managing your health. Incorporating lifestyle changes such as regular exercise, a balanced diet rich in antioxidants, and mental stimulation through activities like puzzles or reading can enhance brain health and potentially offset some risks associated with medication stacking.
By focusing on overall wellness alongside proper medication management, you can create a more balanced approach to maintaining cognitive function as you age.
Recognizing the Signs of Medication Stacking in Older Adults
Recognizing the signs of medication stacking in older adults is crucial for early intervention and prevention of cognitive decline. Common indicators include increased confusion, memory lapses, difficulty concentrating, or changes in mood and behavior. If you notice these symptoms in yourself or a loved one who is taking multiple medications, it’s essential to seek professional guidance promptly.
Additionally, watch for physical signs such as dizziness or falls, which may indicate adverse reactions to stacked medications. Being vigilant about these symptoms allows you to address potential issues before they escalate into more significant health concerns. Engaging family members or caregivers in this process can also provide additional support in monitoring changes in behavior or cognition related to medication use.
The Impact of Medication Stacking on Cognitive Decline
The impact of medication stacking on cognitive decline cannot be overstated; research consistently shows a correlation between polypharmacy and increased rates of dementia among older adults. As you accumulate more prescriptions over time, the likelihood of experiencing cognitive decline rises significantly due to the compounded effects of various medications on brain function. Moreover, cognitive decline resulting from medication stacking often manifests gradually, making it challenging to identify until significant impairment has occurred.
This underscores the importance of proactive monitoring and management of your medications throughout life. By staying informed about how different drugs interact with one another and their potential long-term effects on cognition, you can take steps to protect your brain health as you age.
Seeking Professional Help for Medication Management and Dementia Risk
If you are concerned about medication stacking and its implications for dementia risk, seeking professional help is a critical step toward safeguarding your cognitive health. Engaging with a geriatrician or a pharmacist specializing in elderly care can provide valuable insights into managing complex medication regimens effectively. These professionals can conduct thorough reviews of your current prescriptions and recommend adjustments that prioritize both safety and efficacy.
Additionally, consider involving family members or caregivers in discussions about your medications; their perspectives can help identify any concerns that may arise from daily use. By working collaboratively with healthcare providers and loved ones, you can create a comprehensive plan that addresses both your medical needs and cognitive health goals—ultimately reducing the risks associated with medication stacking while promoting overall well-being as you age.
Recent studies have highlighted the potential risks associated with medication stacking, particularly in older adults, and its connection to increased dementia risk. For more insights on this topic, you can read a related article that discusses the implications of polypharmacy in senior health at Explore Senior Health. Understanding the effects of multiple medications is crucial for managing health in aging populations.
FAQs
What is medication stacking?
Medication stacking refers to the practice of taking multiple medications simultaneously, often without proper coordination or oversight. This can lead to increased risks of drug interactions and side effects.
How can medication stacking affect dementia risk?
Medication stacking may increase the risk of cognitive decline and dementia due to potential adverse drug interactions, increased side effects, and the cumulative impact of certain medications on brain function.
Which types of medications are commonly involved in medication stacking related to dementia risk?
Medications such as anticholinergics, benzodiazepines, and certain sedatives are often implicated because they can impair cognitive function, especially when taken together or in high doses.
Is medication stacking more common in older adults?
Yes, older adults are more likely to experience medication stacking due to multiple chronic conditions requiring various prescriptions, increasing the risk of adverse effects including cognitive impairment.
Can medication stacking be prevented or managed?
Yes, medication stacking can be managed by regular medication reviews with healthcare providers, careful monitoring of drug interactions, and deprescribing unnecessary medications when appropriate.
What should patients do if they are concerned about medication stacking and dementia risk?
Patients should consult their healthcare providers to review all current medications, discuss potential risks, and explore safer alternatives or adjustments to reduce the risk of cognitive decline.
Are there any studies linking medication stacking directly to dementia?
Several studies have found associations between polypharmacy, especially involving certain drug classes, and increased dementia risk, though causation is complex and influenced by multiple factors.
Does medication stacking only affect dementia risk, or are there other health concerns?
Medication stacking can lead to various health issues beyond dementia risk, including falls, hospitalizations, adverse drug reactions, and decreased overall quality of life.