Blood pressure is a critical indicator of your cardiovascular health, reflecting the force exerted by circulating blood against the walls of your arteries. It is measured in millimeters of mercury (mmHg) and is expressed as two numbers: systolic pressure over diastolic pressure. The systolic number, which is the first and higher value, represents the pressure in your arteries when your heart beats.
The diastolic number, the second and lower value, indicates the pressure in your arteries when your heart rests between beats. Understanding these numbers is essential for recognizing how well your heart and blood vessels are functioning. As you age, your blood pressure can change due to various factors, including lifestyle, diet, and underlying health conditions.
It’s crucial to grasp the significance of these changes, as they can have profound implications for your overall health. High blood pressure, or hypertension, can lead to serious complications such as heart disease and stroke, while low blood pressure can cause dizziness and fainting. By understanding what blood pressure means and how it affects your body, you can take proactive steps to maintain a healthy range.
Key Takeaways
- Monitoring blood pressure is crucial for seniors 65+ to prevent health complications.
- Both high and low blood pressure pose significant risks for older adults.
- Lifestyle changes, such as diet and exercise, play a key role in managing blood pressure.
- Medications may be necessary but should be carefully managed under medical supervision.
- Regular doctor visits and home monitoring are essential for effective blood pressure control in seniors.
Importance of Blood Pressure Monitoring for Seniors
For seniors, regular monitoring of blood pressure is vital. As you age, your body undergoes numerous changes that can affect cardiovascular health. Regular checks can help you identify any fluctuations in your blood pressure early on, allowing for timely intervention if necessary.
This proactive approach can significantly reduce the risk of severe health issues down the line. By keeping track of your blood pressure, you empower yourself to make informed decisions about your health and lifestyle. Moreover, monitoring blood pressure can provide valuable insights into how well your current treatment plan is working.
If you are on medication or have made lifestyle changes to manage your blood pressure, regular readings can help you and your healthcare provider assess the effectiveness of these strategies. This ongoing dialogue about your health can lead to adjustments that better suit your needs, ensuring that you remain in control of your well-being.
Current Blood Pressure Guidelines for Seniors 65+

The current guidelines for blood pressure management in seniors aged 65 and older recommend maintaining a systolic blood pressure below 130 mmHg and a diastolic pressure below 80 mmHg. These targets are designed to minimize the risk of cardiovascular events while considering the unique physiological changes that occur with aging. It’s essential to recognize that these guidelines may vary based on individual health conditions and risk factors, so personalized recommendations from your healthcare provider are crucial.
If your readings consistently fall outside these ranges, it may be time to discuss potential lifestyle changes or medication options with your doctor. Being aware of these benchmarks not only helps you stay informed but also encourages you to take an active role in managing your health.
Factors Affecting Blood Pressure in Seniors
Several factors can influence blood pressure in seniors, making it essential to consider both internal and external elements. Age-related changes in blood vessels, such as stiffness and reduced elasticity, can contribute to increased blood pressure. Additionally, chronic conditions like diabetes or kidney disease can further complicate blood pressure regulation.
Understanding these factors allows you to recognize why your readings may fluctuate and what steps you can take to mitigate these influences. Lifestyle choices also play a significant role in blood pressure management. Diet, physical activity, stress levels, and sleep quality all contribute to how your body regulates blood pressure.
For instance, a diet high in sodium can lead to elevated blood pressure, while regular exercise can help lower it. By being mindful of these factors and making conscious choices, you can positively impact your blood pressure readings.
Risks of High Blood Pressure in Seniors
| Age Group | Blood Pressure Category | Systolic (mm Hg) | Diastolic (mm Hg) | Guideline Notes |
|---|---|---|---|---|
| 65 and older | Normal | < 120 | < 80 | Maintain healthy lifestyle; routine monitoring recommended |
| 65 and older | Elevated | 120-129 | < 80 | Lifestyle modifications advised; monitor regularly |
| 65 and older | Hypertension Stage 1 | 130-139 | 80-89 | Consider medication based on cardiovascular risk; lifestyle changes essential |
| 65 and older | Hypertension Stage 2 | ≥ 140 | ≥ 90 | Medication usually recommended; close monitoring required |
| 65 and older | Hypertensive Crisis | > 180 | > 120 | Seek immediate medical attention |
High blood pressure poses significant risks for seniors, as it can lead to various serious health complications. One of the most concerning risks is cardiovascular disease, which includes heart attacks and strokes. When blood pressure remains elevated over time, it puts extra strain on your heart and arteries, increasing the likelihood of damage to these vital organs.
This risk is compounded by other age-related factors, making it crucial for seniors to monitor their blood pressure closely.
The kidneys play a vital role in filtering waste from the bloodstream, and elevated blood pressure can impair their function over time.
Similarly, studies have shown a link between hypertension and an increased risk of dementia. By understanding these risks, you can appreciate the importance of maintaining healthy blood pressure levels and take proactive steps to protect your overall health.
Risks of Low Blood Pressure in Seniors

While high blood pressure often garners more attention, low blood pressure—known as hypotension—can also pose significant risks for seniors. When blood pressure drops too low, it can lead to symptoms such as dizziness, fainting, and fatigue. These symptoms can increase the risk of falls and injuries, which are particularly concerning for older adults who may already be at risk for fractures or other complications.
Low blood pressure can result from various factors, including dehydration, certain medications, or underlying health conditions such as heart problems or endocrine disorders. It’s essential to recognize the signs of hypotension and discuss any concerns with your healthcare provider. By understanding the potential risks associated with low blood pressure, you can take steps to ensure that you maintain a healthy balance.
Lifestyle Changes to Manage Blood Pressure
Making lifestyle changes is one of the most effective ways to manage blood pressure naturally. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can significantly impact your readings. Reducing sodium intake is particularly important; aiming for less than 2,300 mg per day—or even lower if recommended by your doctor—can help lower blood pressure levels.
Incorporating regular physical activity into your routine is another powerful tool for managing blood pressure. Aim for at least 150 minutes of moderate aerobic exercise each week, such as walking or swimming. Additionally, practices like yoga or tai chi can help reduce stress levels, which is beneficial for overall cardiovascular health.
By making these lifestyle adjustments, you not only improve your blood pressure but also enhance your overall quality of life.
Medications for Managing Blood Pressure in Seniors
For some seniors, lifestyle changes alone may not be sufficient to manage blood pressure effectively. In such cases, medications may be necessary to help achieve target levels. There are various classes of antihypertensive medications available, including diuretics, ACE inhibitors, beta-blockers, and calcium channel blockers.
Each class works differently to lower blood pressure and may be prescribed based on individual health needs and conditions. It’s essential to work closely with your healthcare provider when considering medication options. They will evaluate your overall health status and any other medications you may be taking to determine the best course of action.
Regular follow-ups will allow for adjustments as needed to ensure optimal management of your blood pressure while minimizing potential side effects.
Monitoring and Managing Blood Pressure at Home
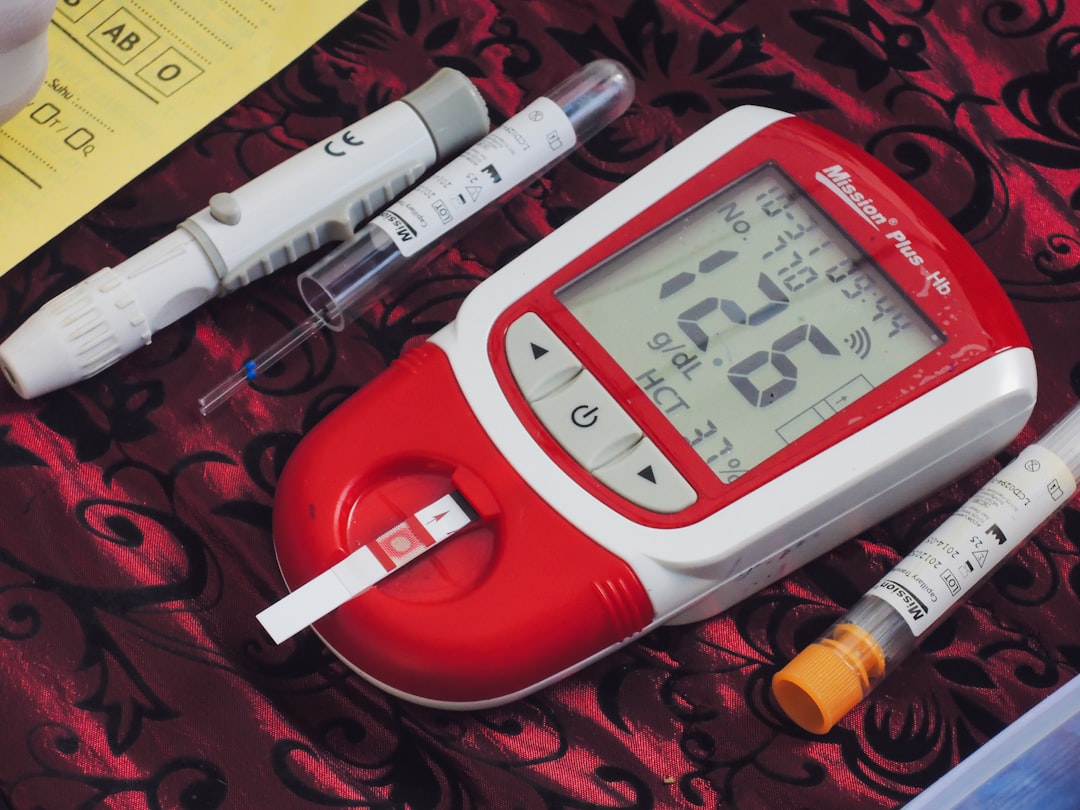
Monitoring your blood pressure at home is an excellent way to stay informed about your cardiovascular health between doctor visits. Home blood pressure monitors are widely available and easy to use; they allow you to track your readings regularly and share this information with your healthcare provider during appointments. Keeping a log of your readings can help identify patterns or triggers that may affect your blood pressure.
When measuring at home, it’s important to follow specific guidelines for accuracy. Ensure that you are seated comfortably with your back supported and feet flat on the floor; avoid caffeine or smoking before taking a reading. Consistency is key—try to measure at the same time each day under similar conditions for the most reliable results.
Importance of Regular Doctor Visits for Blood Pressure Management
Regular doctor visits are crucial for effective blood pressure management in seniors. These appointments provide an opportunity for comprehensive evaluations of your cardiovascular health and allow for adjustments in treatment plans as needed. Your healthcare provider will assess not only your blood pressure readings but also other factors such as weight, cholesterol levels, and overall well-being.
During these visits, don’t hesitate to discuss any concerns or symptoms you may be experiencing related to blood pressure management. Open communication with your healthcare team ensures that you receive personalized care tailored to your unique needs. Regular check-ups also foster a collaborative approach to managing your health—empowering you to take an active role in maintaining optimal blood pressure levels.
Taking Control of Blood Pressure in Seniors 65+
Taking control of blood pressure is essential for seniors aged 65 and older who wish to maintain their health and quality of life. By understanding what influences blood pressure and recognizing the importance of monitoring it regularly, you empower yourself to make informed decisions about your well-being. Whether through lifestyle changes or medication management, there are numerous strategies available to help you achieve healthy blood pressure levels.
Ultimately, staying proactive about your cardiovascular health involves a combination of self-awareness, regular medical check-ups, and open communication with healthcare providers. By taking these steps seriously and prioritizing your health, you can significantly reduce the risks associated with both high and low blood pressure—leading to a healthier and more fulfilling life as you age.
For seniors aged sixty-five and older, managing blood pressure is crucial for maintaining overall health. A related article that provides valuable insights and guidelines for this demographic can be found at Explore Senior Health. This resource offers comprehensive information on the importance of regular monitoring and lifestyle adjustments to help seniors maintain optimal blood pressure levels.
FAQs
What are the recommended blood pressure targets for seniors aged 65 and older?
For most seniors aged 65 and older, the general guideline is to maintain a blood pressure below 130/80 mm Hg. However, individual targets may vary based on overall health, presence of other medical conditions, and a healthcare provider’s assessment.
Why is managing blood pressure important for seniors?
Managing blood pressure in seniors is crucial because high blood pressure increases the risk of heart disease, stroke, kidney problems, and cognitive decline. Proper control helps reduce these risks and improves quality of life.
How often should seniors have their blood pressure checked?
Seniors should have their blood pressure checked at least once every 3 to 6 months if it is well controlled. More frequent monitoring may be necessary if blood pressure is elevated or if medications are being adjusted.
Are there different blood pressure guidelines for seniors compared to younger adults?
While the general target of below 130/80 mm Hg applies to most adults, some guidelines suggest slightly higher targets for very elderly or frail seniors to avoid side effects from aggressive treatment. Individualized care is important.
What lifestyle changes can help seniors manage their blood pressure?
Seniors can manage blood pressure through a healthy diet (such as the DASH diet), regular physical activity, maintaining a healthy weight, limiting salt intake, avoiding excessive alcohol, and quitting smoking.
Can blood pressure medications have different effects in seniors?
Yes, seniors may be more sensitive to blood pressure medications and may experience side effects such as dizziness or falls. Medication regimens should be carefully managed and regularly reviewed by healthcare providers.
When should a senior seek medical advice about their blood pressure?
Seniors should seek medical advice if their blood pressure readings are consistently above recommended targets, if they experience symptoms like headaches, dizziness, chest pain, or if they have concerns about medication side effects.
Are home blood pressure monitors reliable for seniors?
Home blood pressure monitors can be reliable if used correctly. Seniors should be trained on proper measurement techniques and should bring their devices to medical appointments to verify accuracy.