Diphenhydramine is an antihistamine medication commonly sold under the brand name Benadryl. It has been utilized for many years to treat symptoms of allergies, hay fever, and common cold, including sneezing, runny nose, and itchy eyes. Additionally, due to its sedative effects, diphenhydramine is frequently used as a sleep aid.
Many individuals use this over-the-counter medication for symptom relief without considering potential long-term health consequences. Understanding diphenhydramine’s mechanism of action and its broader health implications is important for informed medication use. While it provides immediate symptom relief, recent scientific research has raised concerns about possible associations between extended diphenhydramine use and cognitive decline, particularly among elderly populations.
This information examines these concerns thoroughly to provide a complete overview of diphenhydramine and its potential risks.
Key Takeaways
- Long-term use of diphenhydramine may increase the risk of developing dementia.
- Diphenhydramine is commonly used for allergies and insomnia but has notable side effects.
- Safer alternatives exist for managing allergies and sleep issues without diphenhydramine.
- Recognizing dementia symptoms early is crucial for timely medical intervention.
- Consulting healthcare professionals is important before using diphenhydramine long-term.
Long-Term Use and Dementia Risk
The conversation surrounding long-term use of diphenhydramine has gained traction in recent years, particularly regarding its association with an increased risk of dementia. As you consider your own use of this medication, it’s crucial to be aware of the findings from various studies that suggest a troubling correlation. Research indicates that individuals who regularly consume anticholinergic medications, including diphenhydramine, may face a heightened risk of developing dementia later in life.
This revelation has prompted many healthcare professionals to reevaluate the recommendations surrounding the use of such medications.
By blocking histamine receptors, it can also interfere with acetylcholine, a neurotransmitter vital for memory and learning. Over time, this disruption may contribute to cognitive decline, making it essential for you to weigh the benefits against the risks if you find yourself relying on diphenhydramine for extended periods.
Understanding Diphenhydramine
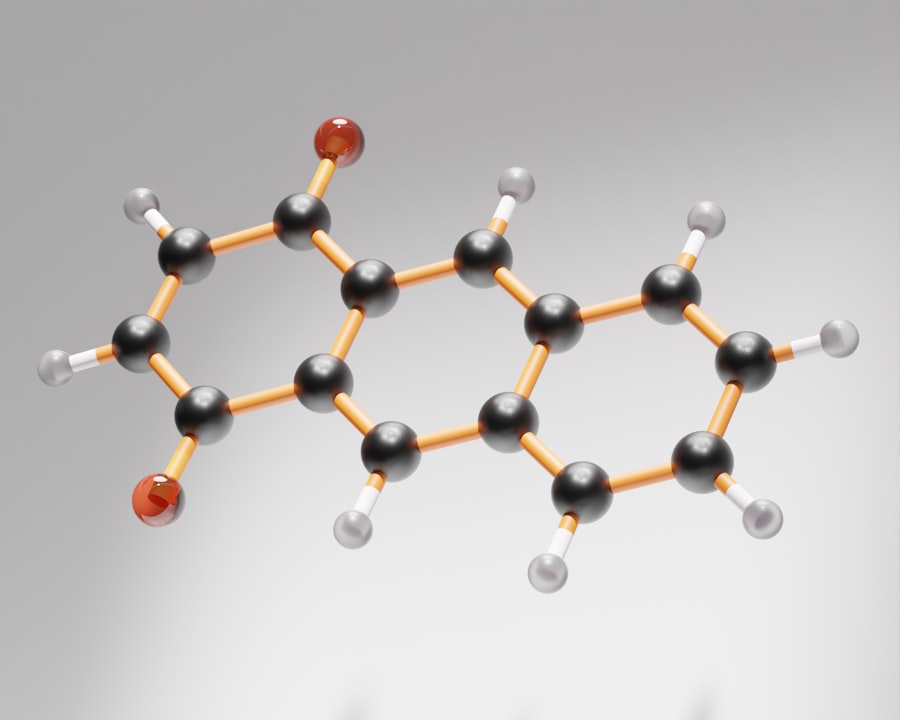
To fully grasp the implications of diphenhydramine use, it’s important to understand how this medication functions within your body. Diphenhydramine is classified as a first-generation antihistamine, which means it can cross the blood-brain barrier and exert sedative effects. When you take diphenhydramine, it binds to histamine receptors in your body, effectively blocking the action of histamine—a chemical responsible for allergic reactions.
This action helps alleviate symptoms like itching and swelling. However, the sedative properties of diphenhydramine can lead to drowsiness and fatigue, which is why many people use it as a sleep aid. While this may seem beneficial in the short term, relying on diphenhydramine for sleep can disrupt your natural sleep cycle and lead to dependence.
As you consider your options for managing allergies or insomnia, it’s vital to recognize that while diphenhydramine can provide immediate relief, it may not be the best long-term solution for your health.
The Link Between Long-Term Use and Dementia
The potential link between long-term diphenhydramine use and dementia is a topic that warrants serious consideration. Studies have shown that individuals who use anticholinergic drugs regularly may experience a decline in cognitive function over time. As you reflect on your own medication habits, it’s essential to recognize that this risk is particularly pronounced in older adults whose cognitive reserves may already be diminished.
The exact nature of this relationship is still being explored by researchers. Some studies suggest that the cumulative effect of anticholinergic medications could lead to changes in brain structure and function over time. This means that if you are using diphenhydramine frequently, you might be inadvertently increasing your risk for cognitive impairment as you age.
Understanding this connection can empower you to make informed decisions about your health and medication choices.
Risks and Side Effects of Diphenhydramine
| Metric | Value | Source/Study | Notes |
|---|---|---|---|
| Increased Dementia Risk | 54% higher risk | Gray et al., JAMA Internal Medicine, 2015 | Long-term use of anticholinergic drugs including diphenhydramine linked to increased dementia risk |
| Duration of Use | >3 years | Gray et al., JAMA Internal Medicine, 2015 | Risk observed with cumulative use over 3 years or more |
| Population Studied | 3,500+ older adults | Gray et al., JAMA Internal Medicine, 2015 | Participants aged 65 and older |
| Anticholinergic Burden Score | High (≥ 3 standardized daily doses) | Campbell et al., 2018 | Higher cumulative anticholinergic exposure linked to cognitive decline |
| Risk Increase per Standardized Daily Dose | 10-20% increase in dementia risk | Campbell et al., 2018 | Incremental risk with each additional standardized daily dose |
| Mechanism | Anticholinergic activity | Multiple studies | Interference with acetylcholine neurotransmission implicated in cognitive decline |
| Recommendation | Avoid long-term use in elderly | American Geriatrics Society Beers Criteria | Diphenhydramine listed as potentially inappropriate for older adults |
While diphenhydramine is generally considered safe for short-term use, it is not without its risks and side effects. As you contemplate using this medication, it’s important to be aware of both common and less common adverse effects. Common side effects include drowsiness, dizziness, dry mouth, and blurred vision.
These effects can impact your daily life, especially if you need to drive or operate machinery after taking the medication. In addition to these immediate side effects, long-term use can lead to more serious health concerns. You may experience increased heart rate or urinary retention, particularly if you have pre-existing conditions such as glaucoma or prostate issues.
It’s crucial to discuss any underlying health conditions with your healthcare provider before starting diphenhydramine or any other antihistamine. Being informed about these risks can help you make better choices regarding your health and well-being.
Alternatives to Diphenhydramine for Long-Term Use

If you find yourself relying on diphenhydramine for allergy relief or sleep assistance, it may be time to explore alternative options that pose fewer risks for long-term use. There are several non-drowsy antihistamines available over-the-counter that do not carry the same cognitive risks as diphenhydramine. Medications such as loratadine (Claritin) or cetirizine (Zyrtec) can provide effective allergy relief without the sedative side effects associated with first-generation antihistamines.
For those struggling with insomnia, lifestyle changes can also play a significant role in improving sleep quality without resorting to medications like diphenhydramine. Establishing a consistent sleep schedule, creating a relaxing bedtime routine, and minimizing screen time before bed can all contribute to better sleep hygiene. By exploring these alternatives, you can reduce your reliance on diphenhydramine while still addressing your health needs effectively.
Managing Allergies and Insomnia Without Diphenhydramine
Managing allergies and insomnia without diphenhydramine requires a multifaceted approach that prioritizes both lifestyle changes and alternative treatments. For allergies, consider incorporating natural remedies such as saline nasal sprays or using an air purifier in your home to reduce allergens in your environment. Additionally, staying hydrated and consuming anti-inflammatory foods can help bolster your immune system and reduce allergy symptoms.
When it comes to insomnia, cognitive behavioral therapy for insomnia (CBT-I) has emerged as an effective treatment option that addresses the underlying causes of sleep disturbances. This therapeutic approach focuses on changing negative thought patterns and behaviors related to sleep, ultimately helping you develop healthier sleep habits without relying on medication. By taking proactive steps in managing your allergies and sleep issues, you can improve your overall quality of life while minimizing potential health risks.
Tips for Safe Use of Diphenhydramine
If you find that you need to use diphenhydramine occasionally, there are several tips you can follow to ensure its safe use. First and foremost, always adhere to the recommended dosage on the packaging or as advised by your healthcare provider. Avoid exceeding the recommended dose or using it for longer than necessary; doing so can increase your risk of side effects and complications.
Additionally, be mindful of potential interactions with other medications you may be taking. It’s essential to inform your healthcare provider about all medications and supplements you are using to avoid adverse reactions. If you experience any concerning side effects while taking diphenhydramine, do not hesitate to reach out to your healthcare provider for guidance.
Recognizing the Symptoms of Dementia
As you consider the potential risks associated with long-term diphenhydramine use, it’s equally important to be aware of the symptoms of dementia. Early recognition can lead to timely intervention and support. Common signs include memory loss that disrupts daily life, difficulty completing familiar tasks, confusion about time or place, and changes in mood or personality.
If you notice any of these symptoms in yourself or a loved one, it’s crucial to seek medical advice promptly. Early diagnosis can provide access to resources and support systems that may help manage symptoms more effectively. Being proactive about cognitive health is essential as you navigate the complexities of medication use and overall well-being.
Seeking Medical Advice for Long-Term Diphenhydramine Use
If you have been using diphenhydramine regularly for an extended period, it’s advisable to consult with your healthcare provider about your usage patterns and any concerns you may have regarding cognitive health. Your provider can help assess your individual situation and recommend alternative treatments or lifestyle changes that may better suit your needs. Open communication with your healthcare provider is key when discussing any medication concerns.
They can provide valuable insights into managing allergies or insomnia without compromising your cognitive health while ensuring that any underlying conditions are addressed appropriately.
Conclusion and Recommendations
In conclusion, while diphenhydramine can offer quick relief from allergy symptoms and serve as a temporary sleep aid, its long-term use raises significant concerns regarding cognitive health and dementia risk. As you consider your options for managing allergies or insomnia, it’s essential to weigh the benefits against potential risks carefully. Exploring alternative treatments and lifestyle changes can empower you to take control of your health while minimizing reliance on medications like diphenhydramine.
Always prioritize open communication with your healthcare provider when making decisions about your health care regimen. By staying informed and proactive about your choices, you can enhance your overall well-being while safeguarding your cognitive health for years to come.
Recent studies have raised concerns about the long-term use of diphenhydramine and its potential link to an increased risk of dementia. For more information on this topic, you can read a related article on senior health at Explore Senior Health. This resource provides valuable insights into the effects of various medications on cognitive health in older adults.
FAQs
What is diphenhydramine?
Diphenhydramine is an over-the-counter antihistamine commonly used to treat allergies, hay fever, cold symptoms, and as a sleep aid due to its sedative effects.
How is diphenhydramine related to dementia risk?
Long-term use of diphenhydramine has been associated with an increased risk of developing dementia, including Alzheimer’s disease, particularly in older adults. This is thought to be due to its anticholinergic properties, which can affect brain function.
What are anticholinergic drugs?
Anticholinergic drugs block the action of acetylcholine, a neurotransmitter involved in memory and learning. Diphenhydramine is an anticholinergic medication, and prolonged use can impair cognitive function.
Who is most at risk of dementia from diphenhydramine use?
Older adults, especially those over 65, are most at risk. The risk increases with higher doses and longer duration of use.
Is short-term use of diphenhydramine safe?
Short-term use of diphenhydramine is generally considered safe for most people. The dementia risk is primarily associated with long-term, regular use.
Are there safer alternatives to diphenhydramine for allergies or sleep?
Yes, there are alternatives with lower anticholinergic effects, such as loratadine or cetirizine for allergies, and non-pharmacological approaches or other medications for sleep. It is advisable to consult a healthcare provider for safer options.
What should I do if I have been using diphenhydramine long-term?
If you have been using diphenhydramine regularly for a long time, especially if you are older, consult your healthcare provider. They can assess your risk and suggest alternative treatments.
Can stopping diphenhydramine reverse dementia risk?
There is no clear evidence that stopping diphenhydramine reverses dementia risk, but discontinuing or reducing use may help prevent further cognitive decline.
How can I reduce my risk of dementia related to medications?
To reduce risk, avoid long-term use of anticholinergic medications like diphenhydramine, use the lowest effective dose for the shortest duration, and discuss medication options with your healthcare provider.
Where can I find more information about diphenhydramine and dementia risk?
Reliable information can be found through healthcare providers, the Alzheimer’s Association, the National Institute on Aging, and peer-reviewed medical literature.
