Bladder urgency is a medical condition characterized by a sudden, intense urge to urinate that is difficult to control. This symptom affects millions of people and can significantly disrupt daily activities, work, and social interactions. The condition often creates anxiety due to the unpredictable nature of the urges and the potential for urinary incontinence.
Several factors contribute to bladder urgency, including advancing age, hormonal fluctuations (particularly in women during menopause), urinary tract infections, bladder stones, neurological disorders, and certain medications. Overactive bladder syndrome is one of the most common underlying causes. Medical conditions such as diabetes, stroke, multiple sclerosis, and Parkinson’s disease can also affect bladder function and increase urgency symptoms.
Bladder urgency frequently occurs alongside other lower urinary tract symptoms, including urinary frequency (urinating more than eight times per day), nocturia (waking at night to urinate), and urgency incontinence (involuntary urine leakage following the urge). Certain dietary factors may exacerbate symptoms, including caffeine, alcohol, artificial sweeteners, spicy foods, and acidic beverages. Stress and anxiety can also intensify bladder urgency through the brain-bladder connection.
Proper medical evaluation is essential for accurate diagnosis and treatment planning. Healthcare providers typically conduct a thorough medical history, physical examination, urinalysis, and may recommend additional tests such as bladder diaries, urodynamic studies, or imaging to determine the underlying cause and develop an appropriate treatment strategy.
Key Takeaways
- Bladder urgency can be managed through various non-anticholinergic approaches beyond medication.
- Behavioral changes and pelvic floor physical therapy are effective first-line treatments.
- Botox injections and neuromodulation offer advanced, drug-free options for symptom relief.
- Complementary therapies like acupuncture, herbal remedies, and cognitive behavioral therapy may support bladder control.
- Combining multiple non-anticholinergic treatments can enhance overall management and improve patient outcomes.
The Limitations of Anticholinergic Medications
Anticholinergic medications have long been a standard treatment for bladder urgency, working by blocking the action of acetylcholine, a neurotransmitter involved in bladder contractions. While these medications can be effective for some individuals, they come with a range of limitations that you should be aware of. One significant drawback is the potential for side effects, which can include dry mouth, constipation, blurred vision, and cognitive impairment.
If you are older or have pre-existing conditions, these side effects may be particularly concerning. Additionally, anticholinergic medications do not address the root causes of bladder urgency; they merely mask the symptoms. This means that while you may experience temporary relief, the underlying issues may persist or even worsen over time.
You might find yourself needing to increase your dosage or switch medications as your body adapts to the treatment. For these reasons, exploring alternative therapies and lifestyle changes can be beneficial in managing bladder urgency more effectively.
Behavioral and Lifestyle Modifications for Managing Bladder Urgency
Making behavioral and lifestyle modifications can significantly improve your experience with bladder urgency. One of the first steps you can take is to establish a regular bathroom schedule. By training your bladder to empty at specific intervals, you may reduce the frequency of urgent urges.
This technique, known as bladder training, involves gradually increasing the time between bathroom visits until you reach a comfortable interval that minimizes urgency. In addition to scheduling bathroom breaks, you might consider keeping a bladder diary. This tool allows you to track your fluid intake, urination patterns, and any instances of urgency or accidents.
By identifying triggers—such as certain foods or drinks—you can make informed choices about what to consume. Reducing caffeine and alcohol intake is often recommended, as these substances can irritate the bladder and exacerbate urgency. Incorporating pelvic floor exercises into your routine can also strengthen the muscles that support bladder control, providing additional benefits.
Pelvic Floor Physical Therapy for Bladder Urgency
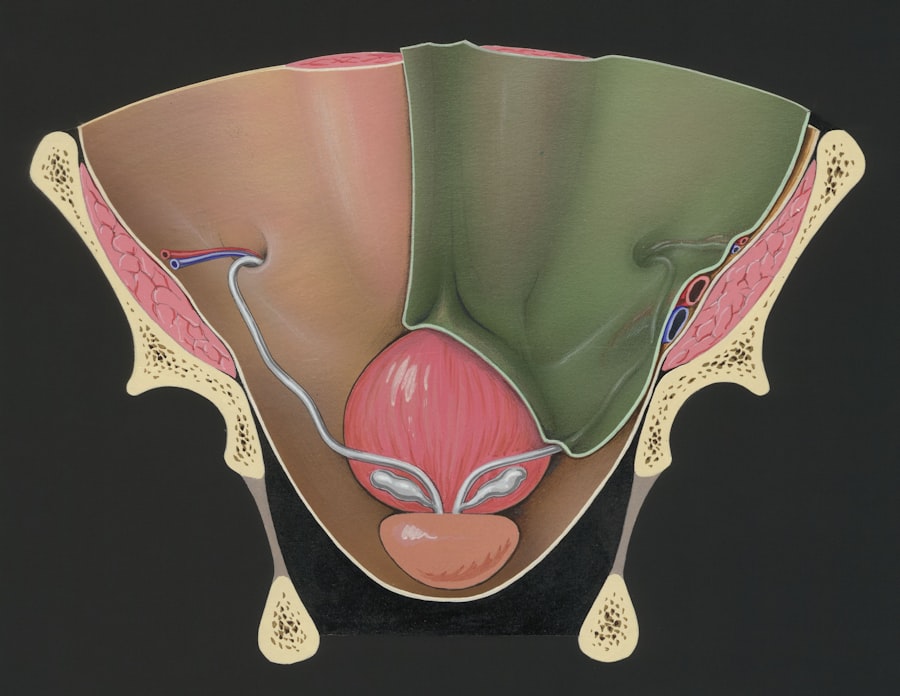
Pelvic floor physical therapy is an effective approach for managing bladder urgency that focuses on strengthening and coordinating the muscles in your pelvic region. A trained physical therapist will guide you through exercises designed to improve muscle tone and control, which can help alleviate symptoms of urgency. You may find that these exercises not only enhance your bladder control but also improve your overall pelvic health.
During therapy sessions, you will learn techniques such as Kegel exercises, which involve contracting and relaxing the pelvic floor muscles. These exercises can be done discreetly throughout your day and require no special equipment.
Additionally, pelvic floor therapy often includes education on posture and body mechanics, which can further support your bladder health.
Botox Injections as a Non-Anticholinergic Treatment Option
| Treatment | Mechanism of Action | Effectiveness | Common Side Effects | Notes |
|---|---|---|---|---|
| Mirabegron (Beta-3 Adrenergic Agonist) | Relaxes detrusor muscle to increase bladder capacity | Moderate to high; reduces urgency episodes by ~30-40% | Hypertension, headache, nasopharyngitis | Non-anticholinergic; suitable for patients intolerant to anticholinergics |
| Botulinum Toxin A (Intravesical Injection) | Inhibits acetylcholine release at neuromuscular junction | High; significant reduction in urgency and frequency | Urinary retention, urinary tract infections | Requires repeat injections every 6-9 months |
| Neuromodulation (Sacral Nerve Stimulation) | Modulates neural pathways controlling bladder function | Moderate to high; improves urgency symptoms in 60-70% of patients | Pain at implant site, infection, lead migration | Invasive; considered after medication failure |
| Pelvic Floor Muscle Training (Physical Therapy) | Strengthens pelvic muscles to improve bladder control | Variable; effective as adjunct therapy | Minimal to none | Non-pharmacologic; recommended as first-line treatment |
Botox injections have emerged as a promising non-anticholinergic treatment option for individuals struggling with bladder urgency. This innovative approach involves injecting small amounts of botulinum toxin directly into the bladder muscle. The toxin works by temporarily paralyzing the muscle, reducing involuntary contractions that lead to urgency and frequency.
If you are seeking an alternative to traditional medications, Botox may provide significant relief. The procedure is typically performed in a healthcare setting and requires minimal downtime. Many patients report experiencing a marked improvement in their symptoms within a few weeks of treatment.
While Botox injections are not a permanent solution—requiring repeat treatments every six to twelve months—they offer a viable option for those who have not found success with other therapies. As with any medical intervention, it’s essential to discuss potential risks and benefits with your healthcare provider.
Neuromodulation for Bladder Urgency

Neuromodulation is another innovative treatment option for managing bladder urgency that involves stimulating nerves responsible for bladder function. One common method is sacral neuromodulation, which involves implanting a small device that sends electrical impulses to the sacral nerves near the lower back. This stimulation helps regulate bladder activity and can significantly reduce symptoms of urgency and frequency.
If you are considering neuromodulation, it’s important to understand that this treatment is typically reserved for individuals who have not responded well to other therapies. The procedure is minimally invasive and can be performed on an outpatient basis. Many patients experience substantial improvements in their quality of life after undergoing neuromodulation therapy.
However, as with any medical procedure, it’s crucial to weigh the potential benefits against any risks involved.
Acupuncture and Traditional Chinese Medicine for Bladder Urgency
Acupuncture and traditional Chinese medicine (TCM) offer holistic approaches to managing bladder urgency that focus on restoring balance within the body. According to TCM principles, bladder issues may arise from imbalances in energy flow or disruptions in organ function. Acupuncture involves inserting thin needles into specific points on the body to stimulate energy flow and promote healing.
If you are open to alternative therapies, acupuncture may provide relief from bladder urgency by addressing underlying imbalances rather than just treating symptoms. Many individuals report experiencing reduced urgency and improved overall well-being after undergoing acupuncture treatments. Additionally, TCM may incorporate herbal remedies tailored to your specific needs, further enhancing the therapeutic effects of acupuncture.
Herbal Remedies and Supplements for Bladder Urgency
Herbal remedies and dietary supplements can also play a role in managing bladder urgency. Certain herbs have been traditionally used to support urinary health and may help alleviate symptoms associated with urgency. For instance, saw palmetto and pumpkin seed extract are often recommended for their potential benefits in promoting bladder function.
Before incorporating any herbal remedies or supplements into your routine, it’s essential to consult with a healthcare professional who can guide you on appropriate dosages and potential interactions with other medications you may be taking. While some individuals find relief through these natural approaches, results can vary widely from person to person.
Cognitive Behavioral Therapy for Bladder Urgency
Cognitive behavioral therapy (CBT) is a psychological approach that focuses on changing negative thought patterns and behaviors associated with bladder urgency. If anxiety or stress exacerbates your symptoms, CBT may help you develop coping strategies to manage these feelings more effectively. Through therapy sessions, you will learn techniques to challenge irrational thoughts related to urination and develop healthier responses to triggers.
CBT can also assist in addressing any emotional distress caused by living with bladder urgency. By fostering a more positive mindset and reducing anxiety surrounding bathroom access, you may find that your symptoms become more manageable over time. Many individuals report improved quality of life after engaging in CBT as part of their overall treatment plan.
The Role of Diet in Managing Bladder Urgency
Your diet plays a significant role in managing bladder urgency, as certain foods and beverages can irritate the bladder or contribute to inflammation. If you are experiencing frequent urges, it may be beneficial to evaluate your dietary choices carefully. Common irritants include caffeine, alcohol, spicy foods, artificial sweeteners, and acidic fruits like citrus.
You might consider keeping a food diary to identify any correlations between what you eat and your symptoms. By eliminating or reducing irritants from your diet, you may experience fewer episodes of urgency and improved overall bladder health. Additionally, staying well-hydrated is essential; however, it’s important to balance fluid intake throughout the day rather than consuming large amounts at once.
Combining Non-Anticholinergic Treatments for Optimal Results
For optimal management of bladder urgency, combining various non-anticholinergic treatments may yield the best results. Each individual’s experience with bladder urgency is unique; therefore, a multifaceted approach allows you to tailor your treatment plan according to your specific needs and preferences. You might find that integrating behavioral modifications with pelvic floor therapy provides significant relief while also addressing underlying muscle issues.
Additionally, exploring complementary therapies such as acupuncture or herbal remedies alongside conventional treatments like Botox or neuromodulation can enhance overall effectiveness. Collaborating closely with your healthcare provider will ensure that all aspects of your treatment plan work harmoniously together, maximizing your chances of achieving lasting relief from bladder urgency. In conclusion, understanding bladder urgency is the first step toward effective management.
While anticholinergic medications have their place in treatment options, exploring alternative therapies such as behavioral modifications, pelvic floor therapy, Botox injections, neuromodulation, acupuncture, herbal remedies, cognitive behavioral therapy, dietary adjustments, and combining these approaches can lead to improved outcomes for those affected by this condition. By taking an active role in your treatment journey and working closely with healthcare professionals, you can regain control over your bladder health and enhance your quality of life.
For those seeking alternatives to anticholinergic medications for managing bladder urgency, a comprehensive overview can be found in the article on non-anticholinergic treatments. This resource discusses various approaches and therapies that may provide relief without the side effects commonly associated with anticholinergics. You can read more about these options in the article available at exploreseniorhealth.
com/sample-page/’>this link.
FAQs
What is non-anticholinergic bladder urgency treatment?
Non-anticholinergic bladder urgency treatment refers to therapies for overactive bladder (OAB) that do not involve anticholinergic medications. These treatments aim to reduce urinary urgency and frequency without the side effects commonly associated with anticholinergic drugs.
Why are non-anticholinergic treatments preferred for some patients?
Non-anticholinergic treatments are preferred for patients who experience side effects from anticholinergic medications, such as dry mouth, constipation, blurred vision, or cognitive impairment. They are also considered for elderly patients or those with contraindications to anticholinergics.
What are common non-anticholinergic treatment options for bladder urgency?
Common non-anticholinergic treatments include beta-3 adrenergic agonists (e.g., mirabegron), behavioral therapies (bladder training, pelvic floor exercises), neuromodulation techniques, and in some cases, botulinum toxin injections.
How does mirabegron work in treating bladder urgency?
Mirabegron is a beta-3 adrenergic receptor agonist that relaxes the detrusor muscle of the bladder during the storage phase, increasing bladder capacity and reducing urgency and frequency without the anticholinergic side effects.
Are there any side effects associated with non-anticholinergic treatments?
Yes, while generally better tolerated, non-anticholinergic treatments can have side effects. For example, mirabegron may cause increased blood pressure, headache, or urinary tract infections. Behavioral therapies have minimal risks but require patient commitment.
Can lifestyle changes help manage bladder urgency without medication?
Yes, lifestyle modifications such as fluid management, avoiding bladder irritants (caffeine, alcohol), weight loss, and timed voiding can help reduce symptoms of bladder urgency and improve treatment outcomes.
Is neuromodulation a non-anticholinergic treatment option?
Yes, neuromodulation therapies like sacral nerve stimulation or percutaneous tibial nerve stimulation modulate nerve signals to the bladder and can reduce urgency symptoms without using anticholinergic drugs.
When should a patient consider non-anticholinergic treatments?
Patients should consider non-anticholinergic treatments if they have contraindications to anticholinergics, experience intolerable side effects, or prefer alternative therapies. A healthcare provider can help determine the best treatment approach.
Are non-anticholinergic treatments effective for all types of bladder urgency?
Effectiveness varies depending on the underlying cause and severity of symptoms. Non-anticholinergic treatments are effective for many patients with overactive bladder but may need to be combined with other therapies for optimal results.
Do non-anticholinergic treatments require a prescription?
Some non-anticholinergic treatments, like mirabegron and botulinum toxin injections, require a prescription and medical supervision. Behavioral therapies and lifestyle changes can often be implemented without a prescription but benefit from professional guidance.
