Bladder urgency is a medical condition characterized by a sudden, intense need to urinate that is difficult to defer. This symptom affects millions of people worldwide and can significantly impact daily functioning, work productivity, and social activities. The condition may lead to urinary incontinence if bathroom facilities are not immediately accessible.
Several physiological factors contribute to bladder urgency. Age-related changes in bladder muscle function and capacity commonly increase urgency symptoms. Hormonal fluctuations, particularly decreased estrogen levels during menopause, can affect bladder tissue elasticity and nerve sensitivity.
Medical conditions including urinary tract infections, overactive bladder syndrome, bladder stones, neurological disorders, and certain medications can also trigger urgency symptoms. Psychological and neurological factors significantly influence bladder urgency. Chronic stress and anxiety can heighten bladder sensitivity through the nervous system’s response mechanisms.
The brain-bladder connection involves complex neural pathways that can become hypersensitive during periods of emotional distress. This creates a physiological cycle where stress increases urgency symptoms, which in turn generates more anxiety about potential incontinence episodes. Identifying specific triggers such as caffeine consumption, fluid intake patterns, stress levels, and environmental factors is essential for developing effective management strategies and treatment plans.
Key Takeaways
- Bladder urgency can be managed through a combination of dietary, lifestyle, and stress management changes.
- Pelvic floor exercises and hydration adjustments play key roles in improving bladder control.
- Herbal remedies, essential oils, acupuncture, and supplements may support bladder health.
- Reducing stress is important for minimizing bladder urgency symptoms.
- Professional medical advice is recommended for persistent or severe bladder urgency issues.
Dietary Changes for Bladder Health
Your diet plays a pivotal role in maintaining bladder health and managing urgency. Certain foods and beverages can irritate the bladder, leading to increased urgency and discomfort. For instance, you may want to limit your intake of caffeine, alcohol, and spicy foods, as these can act as irritants.
Instead, consider incorporating more bladder-friendly options into your meals. Foods rich in fiber, such as fruits, vegetables, and whole grains, can help maintain regular bowel movements and reduce pressure on the bladder. Additionally, staying mindful of your hydration is essential.
You might find it beneficial to establish a hydration schedule that allows you to drink water throughout the day while avoiding excessive intake before bedtime. By making these dietary adjustments, you can create a more supportive environment for your bladder and potentially alleviate some of the urgency you experience.
Herbal Remedies for Bladder Urgency

Herbal remedies have been used for centuries to support various aspects of health, including bladder function. You may find that certain herbs can provide relief from bladder urgency and promote overall urinary tract health. For example, cranberry extract is well-known for its ability to prevent urinary tract infections (UTIs), which can contribute to urgency.
Incorporating cranberry juice or supplements into your routine may help reduce the frequency of UTIs and improve your bladder health. Another herb worth considering is pumpkin seed extract, which has been shown to support bladder function and reduce symptoms of urgency. This natural remedy may help strengthen the pelvic floor muscles and improve overall urinary control.
As you explore herbal options, it’s essential to consult with a healthcare professional to ensure that these remedies are appropriate for your specific situation. By integrating herbal solutions into your wellness routine, you may find a natural way to manage bladder urgency effectively.
Lifestyle Modifications to Reduce Bladder Urgency
Making lifestyle modifications can significantly impact your experience with bladder urgency. One of the most effective changes you can implement is establishing a regular bathroom schedule. By training your bladder to empty at specific intervals, you may reduce the frequency of sudden urges.
You might start by noting how often you typically need to urinate and gradually extending the time between bathroom visits. This approach can help retrain your bladder and improve your overall control. In addition to scheduling bathroom breaks, consider evaluating your daily activities for potential triggers of urgency.
For instance, if you notice that certain situations—such as long car rides or crowded events—intensify your need to urinate, you can plan accordingly. You might choose to limit fluid intake before these situations or identify nearby restrooms in advance. By being proactive about your lifestyle choices, you can create an environment that minimizes the impact of bladder urgency on your daily life.
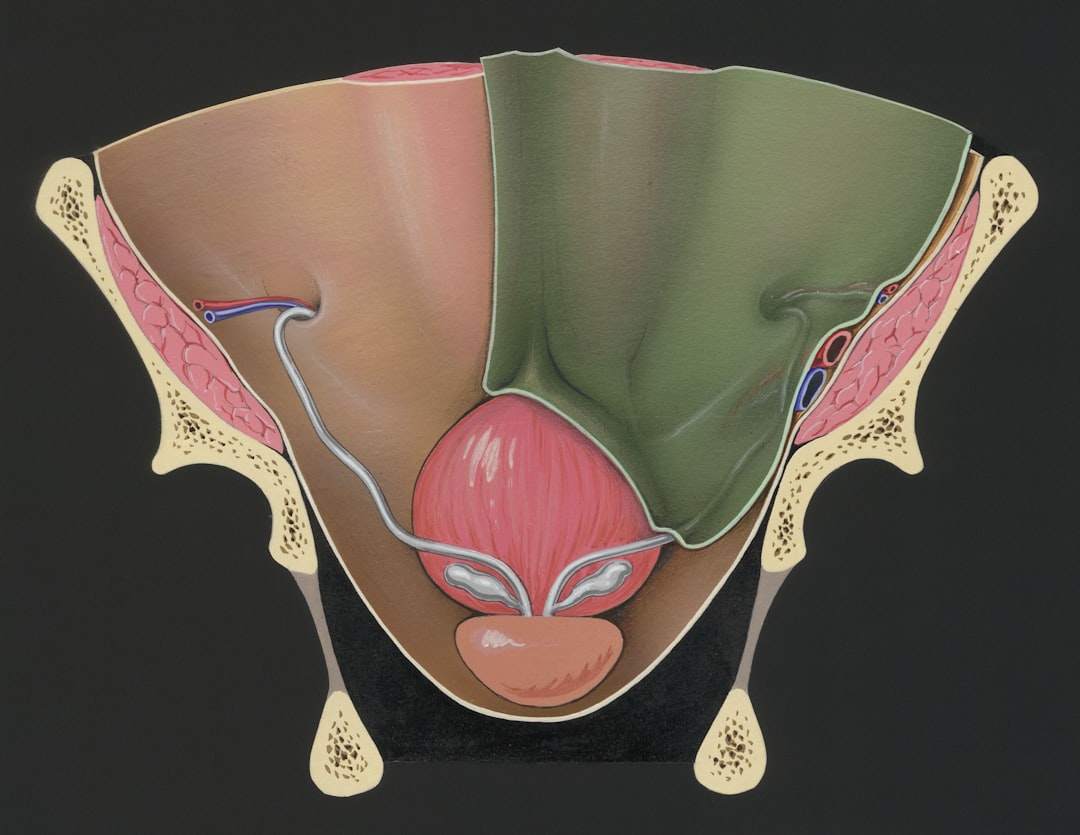
Pelvic Floor Exercises for Bladder Control
| Treatment | Mechanism of Action | Effectiveness | Common Side Effects | Notes |
|---|---|---|---|---|
| Mirabegron (Beta-3 Adrenergic Agonist) | Relaxes detrusor muscle to increase bladder capacity | Moderate to high; reduces urgency episodes by ~30-40% | Hypertension, headache, nasopharyngitis | Non-anticholinergic; suitable for patients intolerant to anticholinergics |
| Botulinum Toxin A (Intravesical Injection) | Inhibits acetylcholine release at neuromuscular junction | High; significant reduction in urgency and frequency | Urinary retention, urinary tract infections | Minimally systemic; requires repeat injections every 6-9 months |
| Neuromodulation (Sacral Nerve Stimulation) | Modulates neural pathways controlling bladder function | Moderate to high; improves urgency symptoms in refractory cases | Pain at implant site, infection, lead migration | Invasive; used when medications fail |
| Behavioral Therapy (Bladder Training) | Improves bladder control through scheduled voiding and urge suppression | Variable; effective as adjunct therapy | None | First-line non-pharmacologic treatment |
Pelvic floor exercises, commonly known as Kegel exercises, are an effective way to strengthen the muscles that support the bladder and improve urinary control. You may find that incorporating these exercises into your daily routine can lead to significant improvements in bladder urgency over time. To perform Kegels, start by identifying the right muscles—these are the ones you would use to stop urination midstream.
Once you’ve located them, contract these muscles for a few seconds before relaxing them. Aim for several repetitions throughout the day. Consistency is key when it comes to pelvic floor exercises.
You might set reminders on your phone or incorporate them into other daily activities, such as while watching television or during your commute. Over time, strengthening these muscles can enhance your ability to control urges and reduce instances of leakage. As you commit to this practice, you may notice not only improvements in bladder control but also an overall sense of empowerment regarding your body.
Stress Management Techniques for Bladder Health

Stress management is an often-overlooked aspect of maintaining bladder health. The connection between stress and bladder urgency is well-documented; when you’re stressed or anxious, your body may respond with increased urgency or frequency of urination.
Mindfulness practices such as meditation or deep breathing exercises can help calm your mind and body, potentially alleviating some of the pressure on your bladder. You might also explore physical activities like yoga or tai chi, which not only promote relaxation but also encourage better body awareness and control over bodily functions. Engaging in regular exercise can help reduce overall stress levels while improving circulation and muscle tone—factors that contribute positively to bladder health.
By prioritizing stress management techniques, you can create a more balanced state of mind that supports better bladder function.
Hydration and Bladder Urgency
Hydration is a double-edged sword when it comes to bladder urgency; while it’s essential for overall health, excessive fluid intake can exacerbate urgency symptoms. Striking the right balance is crucial for managing your condition effectively. You may want to monitor your fluid intake throughout the day and adjust it based on your activity level and individual needs.
Aim for consistent hydration without overwhelming your bladder with large amounts of liquid at once. It’s also important to pay attention to the types of fluids you consume. While water is generally the best choice for hydration, certain beverages—such as those containing caffeine or artificial sweeteners—can irritate the bladder and increase urgency.
You might consider keeping a hydration journal to track how different fluids affect your symptoms over time. By being mindful of both hydration levels and fluid types, you can take significant steps toward reducing bladder urgency.
Essential Oils for Bladder Health
Essential oils have gained popularity for their therapeutic properties, including their potential benefits for bladder health. You may find that certain essential oils can help alleviate symptoms associated with bladder urgency when used appropriately. For instance, lavender oil is known for its calming effects and may help reduce anxiety-related urgency when diffused or applied topically with a carrier oil.
Another essential oil worth exploring is juniper berry oil, which has been traditionally used for its diuretic properties and potential support for urinary tract health. You might consider creating a blend of essential oils tailored to your needs and using it in aromatherapy or topical applications. However, it’s essential to consult with a healthcare professional before using essential oils, especially if you have underlying health conditions or are pregnant.
By incorporating essential oils into your wellness routine thoughtfully, you may discover additional support for managing bladder urgency.
Acupuncture and Acupressure for Bladder Urgency
Acupuncture and acupressure are alternative therapies that have shown promise in addressing various health concerns, including bladder urgency. These practices involve stimulating specific points on the body to promote healing and balance within bodily systems. If you’re open to exploring these modalities, you might find relief from symptoms through targeted treatments aimed at improving urinary function.
Acupuncture involves inserting thin needles into specific points on the body to stimulate energy flow and promote healing. Many individuals report positive outcomes from acupuncture sessions focused on bladder health, experiencing reduced urgency and improved control over time. Alternatively, acupressure allows you to apply pressure to specific points without needles, making it a more accessible option for self-care at home.
By incorporating these techniques into your wellness routine, you may find a holistic approach to managing bladder urgency effectively.
Supplements for Bladder Health
In addition to dietary changes and lifestyle modifications, certain supplements may offer additional support for bladder health and help manage urgency symptoms. You might consider exploring options such as D-mannose, which has been shown to prevent bacteria from adhering to the urinary tract walls—potentially reducing the risk of infections that contribute to urgency. Another supplement worth considering is probiotics, which promote a healthy balance of gut bacteria and may indirectly support urinary health by enhancing immune function.
As with any supplement regimen, it’s crucial to consult with a healthcare professional before adding new products to ensure they align with your individual needs and health goals. By integrating targeted supplements into your routine alongside other strategies, you may enhance your overall approach to managing bladder urgency.
Seeking Professional Help for Bladder Urgency
If you’ve tried various strategies without finding relief from bladder urgency, it may be time to seek professional help. A healthcare provider specializing in urology or pelvic floor health can offer valuable insights into your condition and recommend tailored treatment options based on your unique situation. They may conduct tests or assessments to identify any underlying issues contributing to your symptoms.
In some cases, medication or specialized therapies may be necessary to manage bladder urgency effectively. Your healthcare provider can guide you through available options and help you make informed decisions about your treatment plan. Remember that seeking professional assistance is not a sign of weakness; rather, it’s an empowering step toward reclaiming control over your bladder health and improving your quality of life.
By understanding bladder urgency and exploring various strategies—from dietary changes and herbal remedies to lifestyle modifications—you can take proactive steps toward managing this condition effectively. With patience and persistence, you may find relief from symptoms and enhance your overall well-being.
For those seeking alternatives to anticholinergic medications for managing bladder urgency, a comprehensive resource can be found in the article on Explore Senior Health. This site offers valuable insights into various treatment options that may be more suitable for individuals who experience side effects from traditional anticholinergic therapies.
FAQs
What is non-anticholinergic bladder urgency treatment?
Non-anticholinergic bladder urgency treatment refers to therapies for overactive bladder or urinary urgency that do not involve anticholinergic medications. These treatments aim to reduce bladder spasms and urgency without the side effects commonly associated with anticholinergic drugs.
Why might someone choose non-anticholinergic treatments for bladder urgency?
Some patients may avoid anticholinergic medications due to side effects such as dry mouth, constipation, blurred vision, or cognitive impairment. Non-anticholinergic options can provide symptom relief with potentially fewer or different side effects.
What are common non-anticholinergic treatments for bladder urgency?
Non-anticholinergic treatments include beta-3 adrenergic agonists (e.g., mirabegron), behavioral therapies (bladder training, pelvic floor exercises), neuromodulation techniques, and in some cases, botulinum toxin injections.
How do beta-3 adrenergic agonists work in treating bladder urgency?
Beta-3 adrenergic agonists relax the detrusor muscle of the bladder during the storage phase, increasing bladder capacity and reducing urgency and frequency without blocking acetylcholine receptors.
Are non-anticholinergic treatments effective for all patients with bladder urgency?
Effectiveness varies by individual. Some patients respond well to non-anticholinergic treatments, while others may require combination therapy or alternative approaches. A healthcare provider can help determine the best treatment plan.
What are the potential side effects of non-anticholinergic bladder urgency treatments?
Side effects depend on the specific treatment. For example, beta-3 agonists may cause increased blood pressure or headache, while behavioral therapies have minimal risks. Neuromodulation may involve discomfort or infection risk.
Can lifestyle changes help manage bladder urgency without medication?
Yes, lifestyle modifications such as fluid management, avoiding bladder irritants (caffeine, alcohol), timed voiding, and pelvic floor muscle training can improve symptoms and are often part of non-anticholinergic treatment strategies.
Is botulinum toxin considered a non-anticholinergic treatment for bladder urgency?
Yes, botulinum toxin injections into the bladder muscle reduce overactivity by blocking nerve signals, providing symptom relief without anticholinergic drug use.
Who should consider non-anticholinergic treatments for bladder urgency?
Patients who experience intolerable side effects from anticholinergic drugs, have contraindications to these medications, or prefer alternative therapies may consider non-anticholinergic options after consulting their healthcare provider.
How can I discuss non-anticholinergic bladder urgency treatments with my doctor?
Prepare by noting your symptoms, treatment history, and any side effects experienced. Ask about the benefits and risks of non-anticholinergic options, and whether they are suitable for your specific condition and health status.