As you navigate the complex landscape of Medicare Part D, understanding the significance of plan audits becomes paramount. Part D plans, which provide prescription drug coverage to millions of beneficiaries, are subject to rigorous scrutiny to ensure compliance with federal regulations. These audits serve as a critical mechanism for maintaining the integrity of the program, safeguarding beneficiaries’ access to necessary medications, and ensuring that plans operate within the established guidelines.
By familiarizing yourself with the audit process, you can better appreciate its role in enhancing the quality of care and protecting the interests of both beneficiaries and providers. The audit process is not merely a bureaucratic exercise; it is an essential component of quality assurance in healthcare. Through systematic evaluations, auditors assess whether Part D plans adhere to the standards set forth by the Centers for Medicare & Medicaid Services (CMS).
This oversight helps identify areas for improvement, ensuring that plans deliver on their promises to beneficiaries. As you delve deeper into the intricacies of Part D plan audits, you will uncover the various elements that contribute to a successful audit and the importance of maintaining compliance in this ever-evolving regulatory environment.
Key Takeaways
- Part D Plan audits are essential for ensuring compliance with CMS guidelines and preventing fraud, waste, and abuse.
- Regular audits help in identifying and addressing any discrepancies or non-compliance issues in Part D Plans.
- A comprehensive audit checklist should include reviewing formulary and benefit design compliance, assessing prescription drug event data, and evaluating compliance with CMS guidelines.
- Accuracy and completeness of data are crucial for maintaining compliance and preventing potential issues during audits.
- Documenting audit findings and corrective actions is important for demonstrating compliance and implementing best practices for maintaining compliance.
Understanding Compliance Requirements for Part D Plans
To effectively navigate the audit landscape, it is crucial to grasp the compliance requirements that govern Part D plans. These requirements are designed to ensure that plans operate fairly and transparently while providing beneficiaries with access to necessary medications. The CMS outlines specific guidelines that cover various aspects of plan operations, including formulary management, benefit design, and claims processing.
By understanding these requirements, you can better prepare for audits and ensure that your organization meets the necessary standards. Compliance is not a one-time effort; it requires ongoing attention and commitment. As you familiarize yourself with the regulations, you will discover that they are subject to change, necessitating continuous education and adaptation.
Staying informed about updates from CMS and other regulatory bodies is essential for maintaining compliance. This proactive approach not only helps you avoid potential penalties but also enhances the overall quality of care provided to beneficiaries.
Importance of Conducting Regular Audits
Regular audits are vital for ensuring that Part D plans remain compliant with federal regulations and deliver high-quality services to beneficiaries. These audits serve as a check-and-balance system, allowing organizations to identify potential issues before they escalate into significant problems. By conducting audits on a routine basis, you can uncover discrepancies in claims processing, formulary management, and other operational areas that may affect beneficiaries’ access to medications.
When team members understand that their work will be subject to review, they are more likely to adhere to established protocols and maintain high standards of performance. This culture not only enhances compliance but also improves overall operational efficiency.
As you prioritize regular audits, you will find that they contribute significantly to the long-term success of your Part D plan.
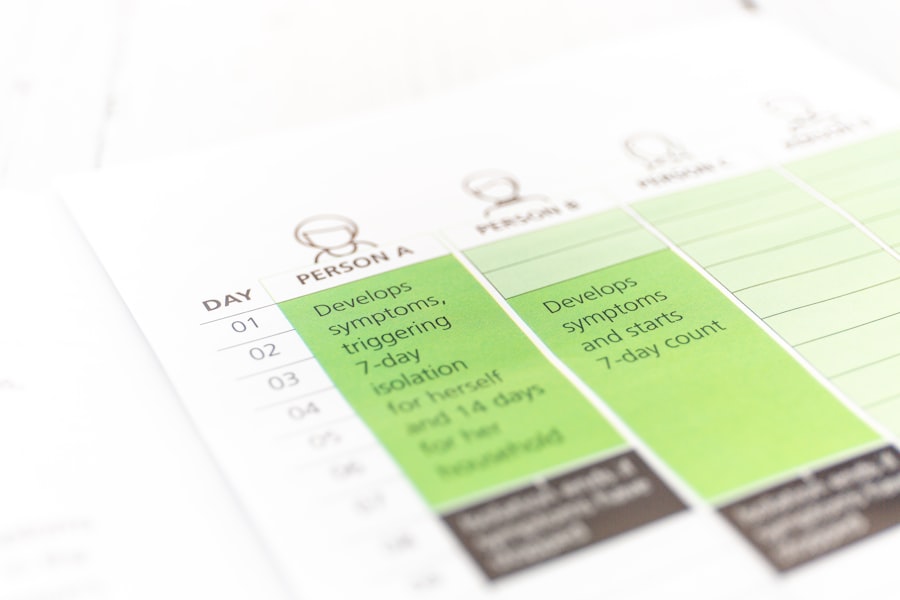
Key Components of a Part D Plan Audit Checklist
| Key Components | Description |
|---|---|
| Beneficiary Eligibility | Verify that the plan has processes in place to ensure that only eligible beneficiaries are enrolled in the plan. |
| Formulary and Benefit Design | Review the formulary and benefit design to ensure compliance with CMS requirements and that it provides adequate coverage for beneficiaries. |
| Utilization Management | Assess the plan’s utilization management processes, including prior authorization and step therapy, to ensure they are being applied appropriately. |
| Pharmacy Network | Examine the plan’s pharmacy network to ensure it provides adequate access to pharmacies for beneficiaries. |
| Compliance Program | Review the plan’s compliance program to ensure it is effective in identifying and addressing compliance issues. |
Creating a comprehensive audit checklist is essential for ensuring that all critical areas are evaluated during the audit process. Your checklist should encompass various components, including compliance with CMS guidelines, formulary management, claims processing accuracy, and beneficiary communication practices. By systematically addressing each area, you can ensure a thorough evaluation that leaves no stone unturned.
In addition to these core components, your checklist should also include provisions for assessing staff training and education. Ensuring that your team is well-versed in compliance requirements and best practices is crucial for maintaining operational integrity. By incorporating these elements into your audit checklist, you can create a robust framework that supports effective audits and drives continuous improvement within your organization.
Ensuring Accuracy and Completeness of Data
Data accuracy and completeness are fundamental to the success of any Part D plan audit. As you prepare for an audit, it is essential to ensure that all data related to claims processing, formulary management, and beneficiary interactions is accurate and up-to-date. Inaccurate or incomplete data can lead to significant compliance issues and may result in penalties or corrective actions from CMS.
To achieve data accuracy, consider implementing robust data management systems that facilitate real-time updates and monitoring. Regularly reviewing data entry processes and conducting internal checks can help identify potential errors before they become problematic. By prioritizing data integrity, you not only enhance your audit readiness but also improve the overall quality of care provided to beneficiaries.
Reviewing Formulary and Benefit Design Compliance
A critical aspect of Part D plan audits involves reviewing formulary and benefit design compliance. The formulary is a list of covered drugs that beneficiaries can access under their plan, and it must adhere to specific guidelines set by CMS. During an audit, you should assess whether your formulary includes all required medications and whether any exclusions are justified based on clinical evidence.
Additionally, evaluating benefit design compliance is essential for ensuring that your plan meets the needs of beneficiaries while adhering to regulatory requirements. This includes examining cost-sharing structures, coverage limitations, and any prior authorization processes in place. By thoroughly reviewing these components during an audit, you can identify areas for improvement and ensure that your plan remains compliant with CMS guidelines.
Assessing Prescription Drug Event Data
Prescription Drug Event (PDE) data plays a crucial role in evaluating the performance of Part D plans. This data captures information about each prescription filled by beneficiaries, including drug costs, patient demographics, and pharmacy details. During an audit, it is essential to assess the accuracy and completeness of PDE data to ensure compliance with reporting requirements.
By analyzing PDE data, you can identify trends in medication utilization and costs, which can inform future formulary decisions and benefit design adjustments. Additionally, discrepancies in PDE data may indicate potential issues with claims processing or beneficiary eligibility. By conducting a thorough assessment of this data during audits, you can enhance your plan’s operational efficiency and ensure compliance with CMS guidelines.
Evaluating Compliance with CMS Guidelines
Compliance with CMS guidelines is at the heart of any successful Part D plan audit. As you conduct your audit, it is essential to evaluate how well your organization adheres to these guidelines across all operational areas. This includes assessing policies and procedures related to claims processing, formulary management, beneficiary communication, and staff training.
To effectively evaluate compliance, consider utilizing a combination of quantitative metrics and qualitative assessments. For example, you might analyze claims processing times or error rates while also conducting interviews with staff members about their understanding of compliance requirements. By taking a comprehensive approach to evaluating compliance with CMS guidelines, you can identify strengths and weaknesses within your organization and develop targeted strategies for improvement.
Addressing Fraud, Waste, and Abuse Prevention
Fraud, waste, and abuse (FWA) pose significant challenges for Part D plans and can have serious consequences for both beneficiaries and organizations. During an audit, it is crucial to assess your organization’s efforts to prevent FWA through robust policies and procedures. This includes evaluating staff training programs on recognizing potential FWA indicators and implementing effective reporting mechanisms.
Additionally, consider conducting data analyses to identify unusual patterns or anomalies in claims submissions that may indicate fraudulent activity. By proactively addressing FWA prevention during audits, you can protect your organization from financial losses while ensuring that beneficiaries receive the medications they need without unnecessary barriers.
Documenting Audit Findings and Corrective Actions
Thorough documentation of audit findings is essential for maintaining compliance and driving continuous improvement within your organization. As you conduct audits, be sure to document all findings clearly and concisely, outlining any areas of non-compliance or opportunities for improvement. This documentation serves as a valuable resource for future audits and helps ensure accountability within your team.
In addition to documenting findings, it is equally important to outline corrective actions taken in response to identified issues. This may include revising policies or procedures, providing additional staff training, or implementing new technology solutions. By maintaining clear records of both findings and corrective actions, you can demonstrate your commitment to compliance and continuous improvement during future audits.
Best Practices for Maintaining Compliance
Maintaining compliance with Part D regulations requires ongoing effort and dedication from all members of your organization. To foster a culture of compliance, consider implementing best practices such as regular training sessions for staff on regulatory updates and compliance requirements. Encouraging open communication about compliance issues can also help create an environment where team members feel comfortable reporting concerns or seeking clarification.
Additionally, consider leveraging technology solutions that streamline compliance processes and enhance data accuracy. Automated systems can help reduce human error in claims processing while providing real-time monitoring capabilities for identifying potential compliance issues. By adopting these best practices, you can create a robust framework for maintaining compliance within your Part D plan while ultimately improving the quality of care provided to beneficiaries.
In conclusion, understanding the intricacies of Part D plan audits is essential for ensuring compliance with federal regulations while delivering high-quality services to beneficiaries. By prioritizing regular audits, creating comprehensive checklists, ensuring data accuracy, reviewing formulary compliance, assessing PDE data, evaluating adherence to CMS guidelines, addressing FWA prevention efforts, documenting findings effectively, and implementing best practices for ongoing compliance maintenance, you position your organization for success in this complex regulatory environment.
A related article that provides valuable insights and resources on this topic can be found at Explore Senior Health. This resource offers guidance on best practices and key considerations for managing Part D plans effectively.
WATCH THIS 🛑 The Medicare Part D Lie That Steals Your $10,000 Drug Savings
FAQs
What is a Part D plan audit checklist?
A Part D plan audit checklist is a tool used by Medicare Part D plan sponsors to ensure compliance with regulations and guidelines set forth by the Centers for Medicare & Medicaid Services (CMS). It includes a list of items that must be reviewed and verified to demonstrate adherence to program requirements.
What is the purpose of a Part D plan audit checklist?
The purpose of a Part D plan audit checklist is to help plan sponsors assess their compliance with CMS regulations and guidelines. It serves as a guide for conducting internal audits and ensures that the plan is meeting the requirements for offering prescription drug coverage to Medicare beneficiaries.
What are some common items included in a Part D plan audit checklist?
Common items included in a Part D plan audit checklist may cover areas such as formulary management, medication therapy management, compliance with marketing guidelines, adherence to beneficiary rights and protections, and accuracy of data submitted to CMS.
Who uses a Part D plan audit checklist?
Part D plan sponsors, including insurance companies and pharmacy benefit managers, use the Part D plan audit checklist to assess their compliance with CMS regulations and guidelines. It is also used by auditors and regulatory agencies to evaluate the performance of Medicare Part D plans.
How often should a Part D plan audit checklist be used?
Part D plan sponsors are required to conduct regular audits to ensure compliance with CMS regulations. The frequency of using the Part D plan audit checklist may vary, but sponsors are expected to perform ongoing monitoring and periodic audits to maintain compliance.