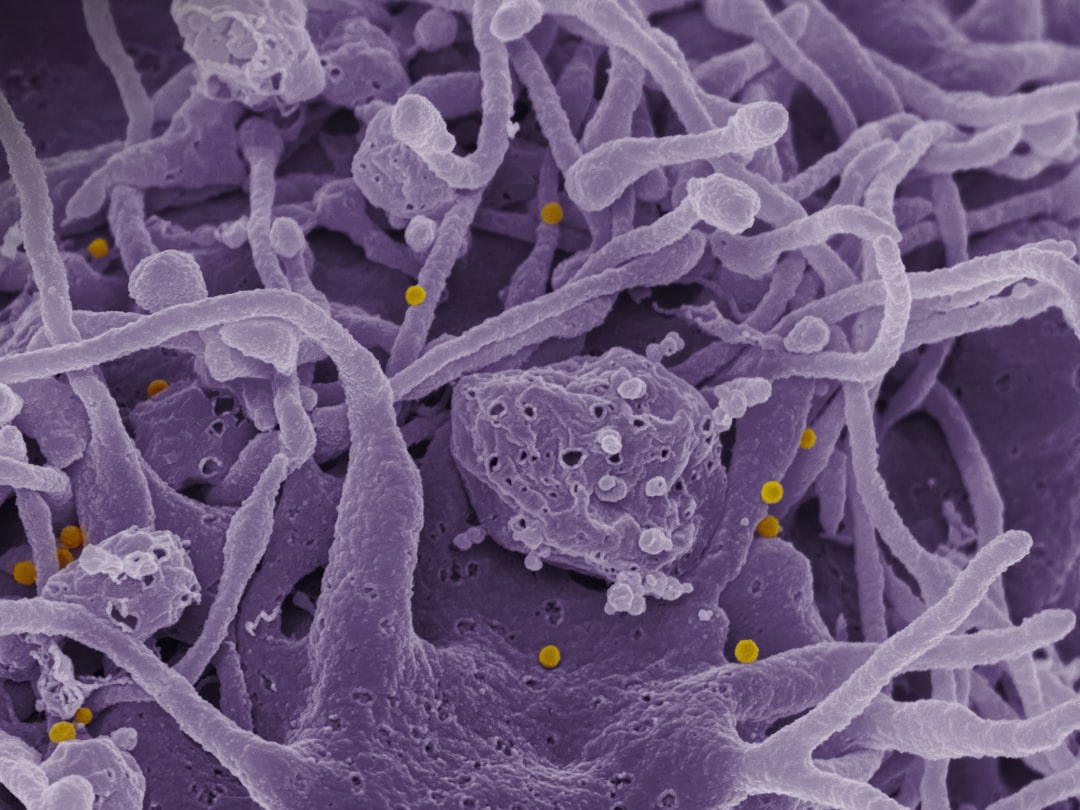
The microbiota-gut-brain axis is a bidirectional communication network connecting the gastrointestinal tract and the central nervous system. This system comprises trillions of microorganisms including bacteria, viruses, and fungi that collectively form the gut microbiome.
Research demonstrates that gut microbiota influence numerous physiological processes beyond digestion, including immune function, metabolism, and neurological processes. These microorganisms synthesize neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), which affect brain function and behavior. Communication between the gut and brain occurs through multiple pathways, including the vagus nerve, immune system signaling, and the production of metabolites and neuroactive compounds.
The composition of gut microbiota can be altered by factors including diet, stress, antibiotics, and environmental exposures. Disruptions to microbial balance (dysbiosis) have been associated with various conditions including irritable bowel syndrome, depression, anxiety, and neurodegenerative disorders. Emerging evidence suggests that interventions targeting gut microbiota composition may provide therapeutic approaches for both gastrointestinal and neuropsychiatric conditions.
Key Takeaways
- The gut microbiota plays a crucial role in maintaining brain health and influencing mental well-being.
- Gut microbes communicate with the brain through biochemical signaling pathways, affecting mood and cognitive functions.
- Imbalances in gut health are linked to neurological disorders and altered stress responses.
- Diet, probiotics, and prebiotics are key strategies to support a healthy microbiota gut-brain axis.
- Ongoing research aims to develop new mental health treatments targeting the gut-brain connection.
The Role of Gut Microbiota in Brain Health
Your gut microbiota serves as a critical player in maintaining brain health. The diverse community of microorganisms in your intestines can influence the production of neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), all of which are essential for regulating mood and emotional well-being. In fact, studies have shown that approximately 90% of serotonin is produced in the gut, highlighting the importance of a healthy microbiome in supporting mental health.
When your gut microbiota is imbalanced, it can lead to disruptions in neurotransmitter production, potentially resulting in mood disorders such as anxiety and depression. Moreover, the gut microbiota also plays a role in neuroinflammation, which is increasingly recognized as a contributing factor to various neurological conditions. An imbalance in gut bacteria can lead to increased intestinal permeability, often referred to as “leaky gut.” This condition allows harmful substances to enter the bloodstream, triggering an inflammatory response that can affect brain function.
By nurturing a healthy gut microbiome, you can help mitigate these inflammatory processes and support optimal brain health.
How Gut Microbes Communicate with the Brain
The communication between gut microbes and the brain occurs through several pathways, including the vagus nerve, immune system signaling, and the production of metabolites. The vagus nerve acts as a direct line of communication between your gut and brain, transmitting signals that can influence mood and behavior. When gut bacteria produce short-chain fatty acids (SCFAs) through the fermentation of dietary fibers, these metabolites can travel through the bloodstream and reach the brain, where they exert neuroprotective effects.
Additionally, your immune system plays a pivotal role in this communication process. Gut microbes can modulate immune responses by producing signaling molecules that influence inflammation levels throughout the body. This immune modulation can impact brain health by either promoting or reducing neuroinflammation.
Understanding these communication pathways is essential for recognizing how changes in your gut microbiota can have far-reaching effects on your mental and emotional well-being.
The Impact of Gut Health on Mental Health
The connection between gut health and mental health is becoming increasingly evident in scientific research. An imbalance in gut microbiota has been linked to various mental health disorders, including anxiety, depression, and even schizophrenia. When your gut microbiome is disrupted, it can lead to alterations in neurotransmitter levels and inflammatory responses that may contribute to these conditions.
As you explore this topic further, you may find that improving your gut health could be a key factor in enhancing your mental well-being. Moreover, lifestyle factors such as diet, stress management, and physical activity can significantly influence your gut microbiota composition. By adopting healthier habits, you can promote a more diverse and balanced microbiome, which may help alleviate symptoms of mental health disorders.
The Influence of Gut Microbiota on Neurological Disorders
| Metric | Description | Relevance to Gut-Brain Axis | Typical Values/Examples |
|---|---|---|---|
| Microbiota Diversity | Variety of microbial species in the gut | Higher diversity is linked to better brain health and mood regulation | Shannon Index: 3-5 in healthy adults |
| Short-Chain Fatty Acids (SCFAs) | Metabolites produced by gut bacteria (e.g., acetate, propionate, butyrate) | Influence brain function by modulating inflammation and neurotransmitter synthesis | Butyrate concentration: 10-20 mM in colon |
| Neurotransmitter Production | Gut bacteria produce neurotransmitters like serotonin, GABA, dopamine | Directly affect mood, anxiety, and cognitive functions | ~90% of body’s serotonin produced in gut |
| Vagus Nerve Activity | Communication pathway between gut and brain | Modulates stress response and emotional regulation | Increased vagal tone linked to reduced anxiety |
| Inflammatory Cytokines | Immune signaling molecules influenced by gut microbiota | Chronic inflammation can impair brain function and mood | IL-6, TNF-alpha levels elevated in dysbiosis |
| Blood-Brain Barrier Integrity | Barrier controlling substance passage to brain | Gut microbiota metabolites help maintain its integrity | Increased permeability linked to neuroinflammation |
Research has begun to uncover the profound influence that gut microbiota can have on neurological disorders such as Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis. These conditions are often characterized by neuroinflammation and neurodegeneration, both of which can be exacerbated by an unhealthy gut microbiome. For instance, studies have shown that individuals with Alzheimer’s disease often exhibit distinct changes in their gut microbiota compared to healthy individuals.
By understanding the role of gut microbiota in these neurological disorders, researchers are exploring potential therapeutic interventions aimed at restoring microbial balance. This could involve dietary modifications or the use of probiotics to promote beneficial bacteria growth. As you consider the implications of this research, it becomes clear that addressing gut health may offer new avenues for preventing or managing neurological disorders.
Gut Microbiota and Stress Response

Your body’s response to stress is intricately linked to your gut microbiota. When you experience stress, your body releases hormones such as cortisol that can impact gut function and microbial composition. Chronic stress can lead to dysbiosis—a state of microbial imbalance—resulting in gastrointestinal issues and further exacerbating stress-related symptoms.
This creates a vicious cycle where stress affects gut health, which in turn influences your ability to cope with stress. Conversely, a healthy gut microbiome can enhance your resilience to stress by modulating the hypothalamic-pituitary-adrenal (HPA) axis—the system responsible for regulating stress responses. Certain beneficial bacteria have been shown to produce metabolites that can help reduce anxiety and improve mood during stressful situations.
By focusing on maintaining a balanced gut microbiome through lifestyle choices, you can potentially improve your stress management capabilities.
The Link Between Gut Health and Cognitive Function
Cognitive function is another area where the health of your gut microbiota plays a significant role. Research suggests that an imbalance in gut bacteria may contribute to cognitive decline and impairments in memory and learning abilities. The production of neurotransmitters and neurotrophic factors by gut microbes is essential for maintaining cognitive function throughout life.
As you age, ensuring a healthy gut microbiome becomes increasingly important for preserving cognitive abilities. Furthermore, studies have indicated that certain dietary patterns rich in fiber, antioxidants, and omega-3 fatty acids can positively influence cognitive function by promoting a diverse gut microbiome. By prioritizing foods that support both gut health and cognitive function, you can take proactive steps toward enhancing your mental acuity and overall brain performance.
Strategies to Support a Healthy Microbiota Gut Brain Axis
Supporting a healthy microbiota-gut-brain axis involves adopting various lifestyle strategies that promote microbial balance. One effective approach is to incorporate a diverse range of whole foods into your diet. Foods rich in fiber—such as fruits, vegetables, whole grains, legumes, nuts, and seeds—can serve as prebiotics that nourish beneficial gut bacteria.
Additionally, fermented foods like yogurt, kefir, sauerkraut, and kimchi provide probiotics that introduce live beneficial bacteria into your system. Regular physical activity is another essential component of maintaining a healthy microbiome. Exercise has been shown to promote microbial diversity while reducing inflammation throughout the body.
Furthermore, managing stress through mindfulness practices such as meditation or yoga can positively impact both your gut health and mental well-being. By integrating these strategies into your daily routine, you can foster a thriving microbiota-gut-brain axis.
The Role of Diet in Maintaining a Healthy Gut Brain Axis
Diet plays a pivotal role in shaping the composition of your gut microbiota and consequently influencing your brain health. A diet high in processed foods, sugars, and unhealthy fats can lead to dysbiosis—a state where harmful bacteria outnumber beneficial ones—resulting in negative effects on both physical and mental health. On the other hand, a balanced diet rich in whole foods supports microbial diversity and promotes optimal functioning of the microbiota-gut-brain axis.
Incorporating foods rich in polyphenols—such as berries, green tea, dark chocolate, and spices—can also benefit your gut health by acting as prebiotics that feed beneficial bacteria. Additionally, omega-3 fatty acids found in fatty fish like salmon or plant-based sources like flaxseeds have been shown to support brain health by reducing inflammation and promoting neurogenesis. By making conscious dietary choices that prioritize whole foods over processed options, you can significantly enhance your gut-brain connection.
The Potential of Probiotics and Prebiotics in Supporting Brain Health
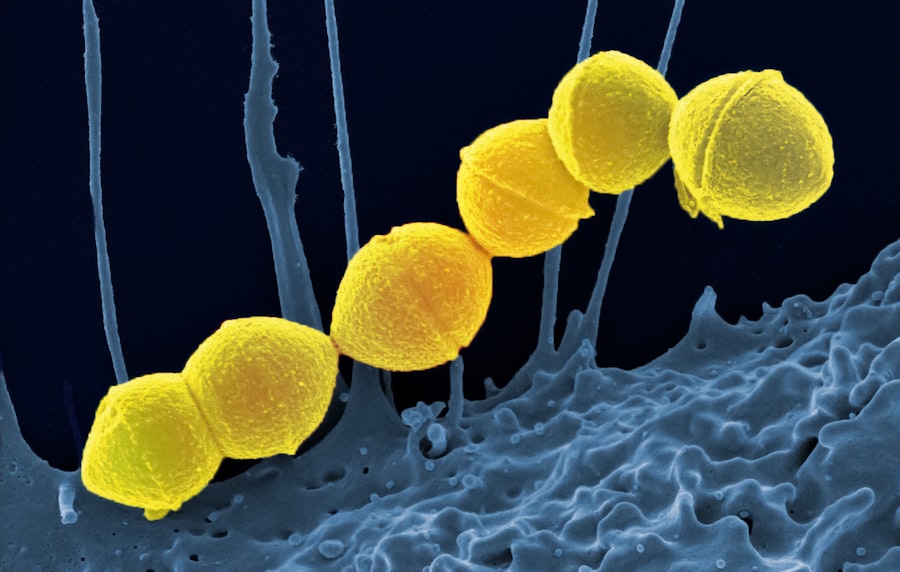
Probiotics and prebiotics are gaining attention for their potential benefits on brain health through their effects on the microbiota-gut-brain axis. Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts; they can help restore balance to an imbalanced microbiome while also producing beneficial compounds that support brain function. Research has shown that specific strains of probiotics may help alleviate symptoms of anxiety and depression by modulating neurotransmitter levels.
Prebiotics—non-digestible fibers found in certain foods—serve as food for beneficial bacteria in your gut. By consuming prebiotic-rich foods like garlic, onions, asparagus, and bananas, you can promote the growth of these beneficial microbes while enhancing their ability to produce metabolites that positively influence brain health. Together, probiotics and prebiotics offer promising avenues for supporting mental well-being through dietary interventions.
Future Research and Implications for Mental Health Treatments
As research continues to unravel the complexities of the microbiota-gut-brain axis, its implications for mental health treatments are becoming increasingly significant. Future studies may lead to personalized approaches for managing mental health disorders based on individual microbiome profiles. This could involve tailored dietary recommendations or targeted probiotic therapies designed to restore balance within the gut microbiome.
Moreover, understanding how lifestyle factors influence the microbiota-gut-brain axis could pave the way for integrative treatment strategies that combine traditional therapies with dietary modifications and lifestyle changes. As you stay informed about ongoing research in this field, you may find new opportunities for enhancing mental health through holistic approaches that prioritize both physical and emotional well-being. In conclusion, the intricate relationship between your gut microbiota and brain health underscores the importance of maintaining a balanced microbiome for overall well-being.
By understanding this connection and implementing strategies to support it—such as adopting a healthy diet, managing stress levels, and considering probiotics—you can take proactive steps toward enhancing both your physical health and mental resilience.
The concept of the microbiota-gut-brain axis has gained significant attention in recent years, highlighting the intricate relationship between our gut microbiome and brain health. For a deeper understanding of this fascinating connection, you can explore a related article on senior health that discusses various aspects of gut health and its impact on overall well-being. Check it out here: Explore Senior Health.
FAQs
What is the microbiota gut-brain axis?
The microbiota gut-brain axis refers to the complex communication network that links the gut microbiota (the community of microorganisms living in the digestive tract) with the brain. This bidirectional system involves neural, hormonal, and immune pathways that influence both gut and brain function.
How does the gut microbiota affect brain function?
Gut microbiota can influence brain function by producing neurotransmitters, modulating immune responses, and affecting the production of metabolites that impact brain chemistry. These interactions can affect mood, cognition, and behavior.
What role does the vagus nerve play in the gut-brain axis?
The vagus nerve is a primary communication pathway between the gut and the brain. It transmits signals from the gut microbiota and the gastrointestinal tract to the brain, helping regulate processes such as digestion, mood, and stress responses.
Can changes in gut microbiota impact mental health?
Yes, alterations in gut microbiota composition have been linked to various mental health conditions, including anxiety, depression, and autism spectrum disorders. Research suggests that maintaining a healthy gut microbiome may support mental well-being.
How do diet and lifestyle influence the gut-brain axis?
Diet and lifestyle significantly affect the composition and diversity of gut microbiota. A diet rich in fiber, fermented foods, and probiotics can promote a healthy microbiome, which in turn supports optimal gut-brain communication and overall health.
Are probiotics beneficial for the gut-brain axis?
Probiotics, which are live beneficial bacteria, may help restore or maintain a healthy gut microbiota balance. Some studies indicate that certain probiotic strains can positively influence mood and cognitive function by modulating the gut-brain axis.
What is the significance of the immune system in the gut-brain axis?
The immune system acts as a mediator in the gut-brain axis by responding to signals from gut microbiota and influencing inflammation levels. Chronic inflammation can affect brain function and has been associated with neurological and psychiatric disorders.
Is the gut-brain axis involved in neurological diseases?
Emerging research suggests that disruptions in the gut-brain axis may contribute to the development or progression of neurological diseases such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis, although more studies are needed to fully understand these connections.
How is research on the microbiota gut-brain axis conducted?
Research involves a combination of animal studies, clinical trials, and microbiome analysis techniques such as DNA sequencing. These methods help scientists understand how gut microbes interact with the nervous system and influence health outcomes.
Can improving gut health enhance cognitive function?
While research is ongoing, evidence suggests that promoting a healthy gut microbiota through diet, probiotics, and lifestyle changes may support cognitive function and protect against cognitive decline. However, individual responses can vary.